|
Newcastle University - Another Graduate Entry !
Dear Kidderminster Medical Society,
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Newcastle University, Year 2 Graduate Entry
I would like to pass on my immense gratitude to Kidderminster Medical Society for your very generous bursary to support me in studying Graduate Medicine at Newcastle University. Having grown up in Kidderminster, it was a great surprise that this organisation existed, and were able to support me in following my medical passion, after graduating from a Masters Degree in Bioengineering from Sheffield University. My first year of GEM consisted of the traditional two years of pre-clinical medicine condensed into a single, slightly extended academic year. In Newcastle there were just 21 students on the graduate course, who I was with for all lectures and seminars. This first year was the most academically challenging and rigorous year of studying I have ever completed. At its conclusion, I was very happy to move to clinical placements where I would be able to start getting real life, hands on experience. As Newcastle is a regional medical school, I spent the year living in Carlilse, which is a nice, large town, reminiscent of Kidderminster! During the year spent there I undertook placements in Emergency and Urgent Care, General Medicine, Surgery, Psychiatry (community and hospital), Paediatrics, Obstetrics and Gynaecology. Carlisle has a relatively small, but incredibly friendly hospital – some of my most memorable experiences were from working on the Labour ward and in the Special Care Baby Unit. Alongside studying I have also been working as a Healthcare Assistant, on the bank, to further support my finances. I have found this job to be a fantastic source of experience in patient care, bedside manner, and working in an interdisciplinary medical team. In particular, I enjoyed working shifts on the Paediatric ward, a specialty that I am very interested in pursuing. Being on placement in Carlilse has also been fantastic for its proximity to the Lake District – I am a keen walker and climber so have managed to fit in a good number of trips this year, which has certainly helped in keeping me grounded and escaping the medical ‘bubble’. A particular highlight was a fantastic weekend training with Patterdale Mountain Rescue team, working alongside their team Doctors, learning about providing medicine in challenging conditions, patient extrication and even signalling to helicopters! I will return to Newcastle this September for my penultimate year, working in the Royal Victoria Infirmary and the Freeman Hospital, before going back to Carlisle for my final year. Thank you again to all members of the Kidderminster Medical Society. Without your generosity I would have struggled with basic financial maintenance, in particular, costs associated with running a car, required to attend placements in GP and rural community settings.
With Grateful Thanks Henry Budden click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
A source of motivation and recognition I am writing to express my heartfelt gratitude for the generous financial grant I recently received from your esteemed organization. This support has significantly impacted my journey as a medical student, and I am sincerely thankful for the opportunities it has provided. Your grant has been instrumental in easing the financial burden associated with pursuing a medical education. It allowed me to acquire essential textbooks, online resources, and materials crucial for my studies. Additionally, it alleviated the strain of tuition fees and living expenses, enabling me to focus on my academic pursuits without constant financial worry. Beyond the financial assistance, your support has been a source of motivation and recognition. Knowing that the Kidderminster Medical Society believes in and supports my educational endeavours has inspired me to strive for excellence. This encouragement has strengthened my commitment to excelling in my studies and contributing meaningfully to the medical field in the future. The impact of the grant extends beyond the classroom, reaching into community service. With your support, I have been able to participate in community health programs and outreach initiatives. These experiences have enriched my education by providing practical, hands-on opportunities to apply classroom knowledge to real-life healthcare scenarios. It is a privilege to give back to the community, and your grant has facilitated my involvement in these valuable endeavours. In conclusion, I want to express my sincere thanks to the Kidderminster Medical Society for investing in my education and future as a medical professional. Your generosity has made a significant difference in my academic pursuits and community service initiatives. I am truly grateful for this opportunity and look forward to contributing to the medical field, inspired by the support you have provided. Thank you once again for your belief in aspiring medical students like myself. Warm regards, Tobias King click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
University of Southampton Graduate Entry Medicine
I would like to extend my heartfelt thanks to the Kidderminster Medical Society for their very generous support during the past academic year. I started my graduate entry medicine studies at the University of Southampton back in September 2022, unaware of what was going to be one of the most challenging but rewarding years of my life. Within the first week we were on the wards taking a history from a new mother and getting to hold an hours-old baby! The whirlwind of the year continued throughout respiratory, cardiac, and GI blocks, ending fittingly on an insightful and powerful week on palliative care. I have thoroughly enjoyed being both on the wards and in the GP surgery, getting first-hand experience of meeting patients and the wider medical team. This September I commenced my second year and in February 2024 we will begin our first full-time placement – something I am looking forward to wholeheartedly. I feel incredibly fortunate to have benefitted from KMS’s bursary scheme which has allowed me to give more time to my studies and enjoy all that this new life venture has to offer. Once again, a massive thank you to Kidderminster Medical Society for their very kind support!
Ellie Ravenscroft
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
As a recipient of the gracious bursary provided by the Kidderminster Medical Society, I am compelled to express my heartfelt gratitude for the invaluable support throughout my preclinical tenure at medical school. This financial aid has relieved the burdens associated with pursuing a graduate course and shaped my educational journey, contributing significantly to my personal and academic growth. My engagement as the President of the Warwick Medic Squash Society has been an enriching chapter of leadership and collaboration. Leading and unifying fellow students has honed my leadership, teamwork, and time management abilities, which I acknowledge as indispensable in medicine. The hands-on exposure during my placement at Warwick Hospital was an enlightening experience. Witnessing real medical scenarios and actively participating in patient care reinforced my dedication to medicine. The interactions with patients and practical application of clinical skills have reaffirmed my aspiration to become a proficient doctor. The accomplishment of passing exams and achieving placement in the 3rd decile for the OSCE is a testament to my diligence and commitment to academic excellence. While I acknowledge areas for further improvement, this milestone has fortified my confidence and proficiency in the medical domain. Crucially, this initial phase has solidified my conviction that medicine is my true calling. The hurdles I’ve surmounted, the lessons learned, and the experiences gained have strengthened my resolve to pursue a career in medicine. The sense of purpose derived from this path fuels my dedication and unwavering commitment to excelling in my studies and profession. My summer immersion in Bogota, teaching English at a science-based bilingual school, was a transformative experience for my personality and language skills. Interacting with diverse cultures and sharing knowledge while taking in wisdom from others was profoundly rewarding. Additionally, establishing connections within the medical community during this period has opened doors for future volunteer opportunities, enabling me to contribute to underserved communities while broadening my medical horizons. I hope to return to Colombia to teach medicine-related topics at my former school and work as a medical professional in a Colombian healthcare setting. None of these accomplishments and enriching experiences would have been feasible without the steadfast support extended by the Kidderminster Medical Society. Your bursary not only eased my financial concerns but also served as a constant source of motivation, urging me to pursue excellence and fulfil my aspirations relentlessly. As I progress into the subsequent years of my medical education, I carry the invaluable lessons, experiences, and encouragement provided through your bursary. I am genuinely thankful for your unwavering support and belief in my potential.
Joshua Clarke click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
From Biomedical Science to Medicine
Without a doubt, the Kidderminster Medical Societies generous bursary allowance has made my transition into studying medicine a truly enjoyable experience. As a mature student with a previous degree in Biomedical Science, returning to university was a daunting prospect, particularly in the financial sense. As tuition fee loans were no longer available being this was my second degree and with maintenance loans being just enough to cover the majority of tuition fees, I was increasingly worried about the cost of living alongside studying the demanding course that medicine is. In truth, searching for financial aid as a mature student proved to be disheartening and the barriers that tuition and living costs pose were and continue to be a huge consideration in my pursuit of becoming a qualified doctor in the future. It is hard to put into words how the bursary the society provided for me has helped in reducing the worries and concerns posed to myself and my family regarding returning to studies. The bursary scheme is something I feel immensely privileged and proud to be a part of – this society is directly investing in the development of future healthcare professionals and can only be held in the highest regard.
With utmost thanks and kind regards Abigail Warren click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Graduate Medicine Bursary Report.
In light of unfortunate circumstances I was required to discontinue my medical studies in the Ukraine and was fortunate enough to recommence them in the UK. The Kidderminster Medical Society bursary has greatly aided me in this transition. I am truly grateful to Dr Lewis and the trustees of the society for their generosity in selecting me and alleviating some financial burden. Their support has truly been invaluable to me. Despite challenges in readjusting from undertaking clinical rotations back to primarily preclinical education, this academic year has been a beneficial review of previous theoretical material which I understand now in far greater depth. As my previous studies had also been affected by the COVID-19 pandemic and anatomy sessions with dissections were no longer routinely possible, the opportunity to carry out full body dissections has been invaluable in thoroughly visualising anatomy. I have also particularly enjoyed teaching other students to learn material by applying methods which had been useful to me previously – in turn acquiring an additional skill. I have found that having been previously familiarised with many of the PBL cases, formulating investigations and management plans in a theoretical setting has strengthened my confidence of relating theory to true cases. I have also been able to identify where I lacked sufficient knowledge and remedy this. Additionally, remote GP placements have been particularly interesting to me as I had been previously unable to undertake them and thus, interacting with patients in primary care was a new experience for me which I greatly benefited from. As I have already covered most of the academic material, I was fortunate to experience a fairly undemanding year, allowing me to invest more time into other interests such as literature writing. For valentines day I also found time to be able to create hand-made cards for some residents at a care facility I had the pleasure to encounter during an ageing and disability placement. Having this extra opportunity and time to connect with people alongside and beyond academic learning, has been truly insightful and heart-warming. I strongly believe that any adversity I have faced will shape me into a more compassionate and resilient clinician. I am truly grateful for having the opportunity to continue my studies and to the society for their support.
Kind Regards Tabia Alam
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Dear Dr Martin Lewis, I hope this letter finds you in the best of health and high spirits. As I sit down to write this, I can hardly believe that my first year of medicine has come to a close. It has been an extraordinary journey, filled with both challenges and triumphs, and I owe much of my success to your incredible generosity and support through the bursary you provided. From the moment I set foot in the medical school, I knew that I had embarked on a path that would test my limits both academically and emotionally. The countless hours of studying, the practical training, and the intense clinical experiences have shaped me into a more resilient and compassionate individual. The opportunity to learn from dedicated lecturers and work alongside medical professionals has been nothing short of inspiring. My first year at medical school focused on building a strong foundation in the basic sciences and medical knowledge. In addition, every Monday we had the opportunity to interact with “PCPIs” (patient, carer and public involvement) which allowed us to develop our communication skills. Your belief in my potential and your willingness to invest in my education have lightened the financial burden that comes with pursuing a career in medicine. Thanks to your bursary, I could focus more on my studies and experiences, allowing me to immerse myself fully in the course without worrying about the financial strain. I was able to achieve a merit, ranking within the top 10% of my cohort. The first year of medicine has solidified my passion for this field, and I am more determined than ever to make a meaningful impact in the lives of patients and contribute to the advancement of healthcare. Your support has played a vital role in fuelling this dedication, and I am truly grateful for the doors of opportunity it has opened for me. Once again, I want to express my sincere gratitude for your unwavering support throughout my first year of medicine.
With heartfelt thanks and warmest regards, Grace Doyle click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
I am writing to wholeheartedly thank you for the support that you provided me through my first year of studying Graduate Entry Medicine at the University of Birmingham. I have just completed my first year of study having passed all of my exams and assessments, and I am excited to progress to my next year of study and to begin my clinical placements in hospitals across the region.
Throughout this intense first year of study I have learnt a great deal and had many opportunities to shadow and learn from some brilliant doctors, nurses and wider allied health professionals both on my GP placement and in University. Although the transition back to studies from working was always going to be a challenge, the bursary has allowed me to fully engage with my studies, massively reducing the number of hours I have needed to work alongside university. This has been invaluable, in hindsight I am unsure how I would have been able to complete this year without this support due to the intensity of the year and the sheer volume of content I had to learn and the time that this took.
I have also managed to use this breathing space afforded to me by the bursary to complete a scheme to train to be a swimming teacher, which will be a sustainable way for me to support myself alongside my studies throughout the remainder of my education, with the added bonus of being a fun part time job that will help me develop skills that will be so useful as a Doctor! Without the support of the bursary, taking the time out of my summer to do this free programme would not have been possible, fortunately I have been able to work part time and do this scheme which will leave me in a good position for the years to come.
I would once again like to thank all of the trustees involved in the decision to give me the bursary, and for the continuation of it to help further students in the future. The support provided has enabled me to get the best foundation of my medical career and for that I am hugely grateful.
Yours,
Megan Larkin click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Graduate Medicine Course at the University of St Andrews
Last year, I moved from Birmingham to start my graduate medicine course at the University of St Andrews. Due to having to wait for my A-level Chemistry result, this left me with only five days’ notice to sell an entire flats worth of belongings, quit my job, say my goodbyes and move up! Additionally, due to the housing crisis, I had to move up with only two suitcases and live on the sofa of two girls I had never met before. I connected with them on a facebook group for our course, and ended up staying on their sofa for a month. Thankfully we have remained close friends ever since, and I found a place of my own to move into.
Moving to Scotland has had its ups and downs…literally; I am very good at walking up hills now. From being in the dissection labs for the first time to seeing patients, this year has been very busy and I am amazed by how much you can learn in such a short space of time. I am looking forward to the next academic year, where I will begin a series of rotations through Dumfries and Galloway, Inverness and various places in Fife. I will have blocks in adult, elderly, palliative, obs and gynae and paediatrics, with the aim being that by the end of the year I should be able to consult anyone walking through the door. The year will end with a 6 week block of emergency medicine, for which I am lucky enough to have been allocated a remote and rural placement which I am very excited for.
I want to thank Kidderminster Medical Society for their generous Graduate Medicine Bursary which has meant I have been able to spend less time working, and more time studying and making friends, and even enjoying a Guinness or two! It has also enabled me to continue activities I enjoy such as hill walking, climbing, and wild swimming to help me relax. This year I was delighted to find that I had been awarded a distinction following such a good work-life balance, and I am aiming for this achievement in further years.
Thank you so much for all your support,
Gemma Peters click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
To the Trustees of the Kidderminster Medical Society Thank you so much for your generous support through the postgraduate bursary during this past academic year. When I found out about this support from the Society, I was so happy that there existed groups which endeavour to support students from our local area to pursue medicine as a career. The decision to study medicine required deep consideration of the balance of investing into what I believed would be a fulfilling career and the financial opportunity cost of further study. I was incredibly fortunate to have been awarded this additional financial support which have tipped these scales in a positive way for me. The academic year has been intense, but I have enjoyed the company of 28 other students who came with a wide variety of backgrounds allowing us to share expertise in our respective previous fields throughout the year. I have spent many days and evenings in the library but have passed all exams on the first take. The bursary from the Society enabled me to get by this year and focus wholly on forming a strong basis of human anatomy and physiology onto which I can build my clinical skills. Having arrived at medical school with a medical research background after completing my PhD at Birmingham and postdoctoral fellowship in the US, I was eager to keep my hand in research. This summer I have joined a lab at Birmingham and have been helping Masters’ and Undergraduate Summer Students to learn new skills in the lab and complete their data collection and analysis. I have always enjoyed getting others into science and hope to continue to do this throughout my medical training. Next year I have joined the committee for Oncology Society and hope to develop networks with local oncologists through this role and learn more about the clinical side of the field in which I hope to build my career. Once again, I am thankful to have received the support of the Kidderminster Medical Society at the start of my medical training.
Best
wishes,
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
A few days into the second half of my 5th year elective, based in rural UK healthcare, when I found myself in the back of a community ambulance, feeling uncomfortably nauseous. The ferry was rolling in all directions as we embarked on an extremely rough inter-island ferry crossing over to mainland Shetland. Our mission was to transfer a patient, one of the 1100 people living on Whalsay, to the local hospital as the lab had reported a Hb level of 42 that morning. As local residents of the island, the 2 voluntary paramedics and the patient chatted cheerfully, yet were taken aback after I declined their offer of sweets for the third time during the crossing. I anxiously deciphered an escape plan in case of the sudden need to find a toilet, a bucket, or the side of the ferry, whilst simultaneously craning my neck in order to not miss an opportunity to sight a whale or an otter through the small porthole (staring at the horizon is one of the first rules of seasickness after all). The view from the ferry, back towards the island of Whalsay (pronounced ‘wallsa’, known as the ‘bonnie isle’) captured everything I had wanted from my elective- a rural placement in a small, tight knit community, which relies on the knowledge, teamwork, and breadth of skills of not just the medical professionals, but the whole Island community. Working closely alongside the team at Whalsay Medical Centre, enabled me to be embedded into the community and really understand the unique provision of healthcare in this truly rural setting. Whalsay, the 6th largest Island of Shetland (not ‘The Shetlands’), is 5 miles long and lies at 60 degrees latitude, x miles off the northern tip of Scotland. A thriving fishing industry, and home to the largest fishing boats in the UK, Whalsay is a wealthy island, yet cut off from the mainland Shetland by a 30-minute ferry crossing. Whalsay Medical Centre is supported by 8 different General Practitioners (GPs) that each stay on the Island for 2-3 weeks at a time, on rotation throughout the year. With no Emergency Department or state funded ambulance provision near, it is the responsibility of the GP on the island at any given time to provide 24-hour medical assistance as required. However, you would be mistaken if you thought this was a solo effort; soon after talking to the receptionists at the health centre and hearing the tales of patients being evacuated via fishing boats in heavy weather, you quickly understand the sense of togetherness that is at the heart of this community. Although the summer months will see many bird watchers and walkers visit Whalsay, and golfers keen to play on the UKs most northerly course, with no hotels or commercial accommodation available, tourists staying overnight on the Island is rare. Luckily, a bit of insider knowledge enabled me to secure a chalet owned by one of the residents on the Island. A brief chat with the owner and I was assured there was somewhere to stay, all be it with no WiFi or Booking.com advertisement to refer to. I headed across on the ferry for the first time, excited and apprehensive about the trip, with instructions to consult the men working on the ferry for directions to the chalet. Dated, yet warm and comfortable, complete with tea cosies and many hot-water bottles, the accommodation was the perfect base. Sitting in the armchair, I had near panoramic over the port of Symbister, the fish farm and hills to the right, and the medical centre just visible at the top of the hill. My commute into the practice was a mere 15-minute walk up the hill, passing a bay which nearly always had 2 or 3 seals playing in the shallows, to arrive shortly before 9am in the morning. Now, one thing that you should know if you are to ever visit the island, or other small island in Shetland, is that it is common courtesy to raise a hand in greeting at every passing car or pedestrian. As big-city, urbanised citizens, it can feel forced and unnatural at first, but it quickly becomes a pleasant part of the day. As it turns out, it is also a difficult habit to get out of, to the horror and bewilderment of fellow commuters around Southmead Hospital in North Bristol. And so, after having made 20 or so new friends on my walk in, I would enter the practice to greet the receptionists, the nurses, and the GP. Days in the clinic passed easily, and although appointments were similar to other village GPs I have been in, clinic lists are a fraction of what you would normally expect, and a much greater proportion of patients are seen as home visits. It was the norm for patients to have same day appointments for non-emergency presentations, and many of the locals have the direct landline to the GPs accommodation on the island for advice out-of-hours. One of the more memorable patients that demonstrated this time-pressured free approach to general practice quite aptly, was a man with multiple sclerosis seen as a home visit. After complaining of difficulty opening his bowels, the GP prescribed some laxatives. Lo and behold, later that afternoon, the GP received a phone call to confirm that the laxatives had done the trick. It was refreshing to see a GP that operated as a true community practitioner, to help with ails and ailments alike, in a world that seemed so far from the stresses of targets and time constraints that seem to monopolise nearly all other GPs. In many ways, Whalsay Medical Centre seems to demonstrate a way of practice that I feel other urbanised communities within the UK are craving for and desperately trying to hold onto. Community care resonated through the relationship between the Medical Centre and the local care home, where the GP will visit to do a mini ward-round roughly every 2 weeks, working closely with the nursing staff and checking in with the patients. During my placement, I was given the responsibility of consulting and examining the patients on my own, before reporting back and accompanying the GP for the more formal review. The care home was a great way to test the progress of my understanding of the Whalsay dialect. Influenced heavily by both Scottish and Scandinavian occupation, the Shetland dialect alone is unique. The Whalsay dialect however, that seems to be preserved by generations on generations remaining on the island, often resulted in me being left completely in the dark during the tales of the morning coffee breaks in the GP practice. None-the-less, the care home was a unique and privileged insight into life for locals on the Island. Culture and tradition on Whalsay are not better demonstrated than through the fishing community, which, as I have already alluded to, is big business on Whalsay. Either through processing, working on fish farms or in the pelagic and white fish fishing boats, many of the young men visiting the GP practice will be often involved in fishing in some form. This presented a few slightly different aspects to GP than a standard mainland centre. Firstly, people involved in fishing often worked in shifts, giving GPs a window of 2-3 weeks in which to diagnose, manage and treat any illnesses or diseases before workers left the island again. Additionally, the GP acts as a lifeline for any Whalsay registered vessels at sea, it is paramount that the GP knows the medical equipment and competencies of the crew on board a vessel to offer support and to help manage casualties remotely. Towards the end of my trip, drawing a sense of completeness and of natural ending to my experience, I visited the lady that I had earlier accompanied over to the mainland in that bumpy ambulance trip. I was happy to see her looking well and eagerly reporting that she is feeling much better following treatment in Gilbert Bain Hospital, which, as a side note, is a very small hospital with no intensive care unit or magnetic resonance scanner. With only 1 medical ward and 1 surgical ward, which contains the 2-bed high dependency unit, if you are going to get really sick on Shetland, expect a swift medical evacuation to Mainland Scotland, weather dependent of course. After 2 short weeks and with a brand-new Fair Isle jumper to commemorate my travels, it was time to return to mainland Scotland via the overnight 13hr North Link ferry to Aberdeen. It is safe to say, that after many years of a self-professed immunity to seasickness, the North Sea and weekly gale-force winds battering Shetland are indeed humbling. I cannot thank the whole team at Whalsay Medical Centre and the community as a whole for their support and welcome, and for making my elective on Whalsay so memorable. I can’t wait to return and continue my quest for a whale sighting.
Brooklyn Clarke click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Nepal Elective Report April-May 2023
Firstly, I would like to thank the Kidderminster Medical Society for the invaluable and generous support for my medical elective to Kathmandu, Nepal. I began my elective on the Easter Bank Holiday at a time that was cold and wet in the UK. In contrast, my arrival in Kathmandu on the Sunday morning was already in excess of 25oC. To say I was overdressed for the heat would be an understatement. However, I was baffled to see all the locals in long sleeves, trousers or long skirts, and even the occasional beanie or hoody. Our Work the World guide instructed us that this was early summer for Nepal and the temperature was in fact cool for them. Within an hour of arriving in Nepal I was already being surprised by the cultural differences.
This brings me nicely on to the TUTH itself. The hospital itself has been operating since 1982 and is the largest hospital in Nepal, with patients travelling across the country to attend. It predominantly operates as a private service, but it is one of the few hospitals in Kathmandu that has governmental subsidies for treatment. However, this subsidy is minimal, and patients’ families must bear the brunt of the cost of healthcare, otherwise known as “out-of-pocket payments”. The doctors would write a list of medicines and items such as cannulas, dressings, and syringes, for the families to purchase at the pharmacies outside the hospital grounds, which the nurses would then administer upon their return. I spent 3 weeks of my elective observing the paediatric team ‘Unit 1’. We would arrive at 9am for an hour’s teaching, which could either be a presentation by primary residents on a topic, a case presentation, or an audit. From these I learned: · Rheumatic fever was still prevalent in country, mostly due to delayed presentation or inability to afford the treatment. · Common but self-resolving skin conditions in neonates. · The effects of chronic kidney disease in the Nepalese paediatric population and the treatments available. Only the affluent could afford a kidney transplant, but dialysis was government funded. · Nepal is much better than the UK in its waiting times for diagnosis of neurodisability such as ADHD and autism but lacks any system to support them beyond diagnosis. · Respiratory support for a pre-term newborn. There were many interesting conditions I saw in both the ward rounds and outpatient appointments. Ward rounds and notes were in English, so it was mostly easy to follow what was going on and therefore understand the conditions I was seeing. Some of the conditions were those commonly seen in the UK, such as gastroenteritis, respiratory conditions such as croup and bronchiolitis, chronic kidney disease, immune thrombocytopenic purpura, autism, Down’s syndrome complications, cancers. However, they were often in a further stage in the disease process or had a poorer outcome. For example, kidney transplants were not commonplace, often only available for the wealthy, with increased likelihood of post-surgical complications due to the lack of proper infection protection and control measures, as well as the affordability of follow-up health care. I was also able to see some other cases not so common to a district paediatric hospital in the UK; malrotation of the gut in a newborn, Kasabach Merritt syndrome, and cardiac symptoms due to rheumatic fever.
However, it was not all doom and gloom on the paediatric front. Nepal exceeds the UK in terms of the uptake of child immunisation programmes, with 6 districts obtaining 99.9% coverage. With almost all the WHO recommended vaccines being issued and fully funded by governmental programmes. The senior doctor in my Unit was keen to educate the other doctors on the importance of providing vaccinations of pneumococcus, influenza, and varicella in the immunocompromised, and highlighting the antibiotic resistant bacteria prevalent in the department and what the treatments should be.
There are no general practice services in Nepal, instead Health Posts are usually government/charity funded positions in rural areas staffed by nurse/midwife practitioners, paramedics, and health care assistants. They can issue vaccinations, basic antibiotics, and provide basic wound care. However, anything more complex required the advice to visit the hospital in Kathmandu. The staff were friendly and deferential, and they were clearly trying to make the best of what they had. All donations of medications from Work the World were received graciously. During my time in Nepal, I found the support from the Work the World staff invaluable to my enjoyment of the placement as well as getting to know their home country. I am unable discuss all of the experiences I had during my four weeks in Nepal, or this would become a novel. Nepal has a rich culture and a medical experience that will remain with me always.
Alexandra Colebrook click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
A Month at the Diving Diseases Research Centre, Plymouth I would like to pass on my sincere thanks to all members of the Kidderminster Medical Society for their very generous elective bursary. This has enabled me to explore an area of medicine which I simply would not have been able to experience otherwise, please see below a brief account of what I was able to get up to. Should any members have any queries or want to know more about what I got up to and diving and hyperbaric medicine in general, I am more than happy to answer any questions and can be contacted at: hegartymk@cardiff.ac.uk. In March 2023 I have been fortunate enough to spend a month at the Diving Diseases Research Centre (DDRC) in Plymouth, a hyperbaric medical facility which offers emergency advice and treatment to patients with diving related illnesses or iatrogenic gas emboli, routine hyperbaric oxygen therapy to patients with a variety of conditions, and medical assessment of commercial and recreational divers, in addition to a wide range of professional training courses. During my time at DDRC I was able to see a large variety of patients ranging from a patient requiring hyperbaric oxygen therapy (HBOT) whilst intubated following iatrogenic venous gas embolism to an elective patient with sudden sensorineural hearing loss. It has been fascinating both learning about the underlying physiology and clinical science behind the use of hyperbaric oxygen and seeing symptomatic improvement in patients for whom there is no other medical intervention able to help them. Whilst DDRC has a contract from the NHS to offer emergency provision of HBOT to certain patients, it maintains a charitable arm which offers treatment to these elective patients for whom the evidence base suggests HBOT could offer some real benefit. This includes patients with slow-healing wounds, postradiotherapy osteoradionecrosis, post-radiotherapy proctitis, sudden sensorineural hearing loss, and necrotising otitis externa – a comprehensive list of conditions for which HBOT is indicated can be seen in the results of the European consensus conference for hyperbaric medicine (Diving and Hyperbaric Medicine, 47(1):24-32. March 2017). Whilst these elective patients provide both good clinical outcomes and serve as great way to maintain staff competencies and maximise use of the facilities, the core of DDRC’s clinical purpose is to treat emergency cases. This predominantly takes the form of divers with decompression illness (DCI). DCI encompasses a broad span of symptoms ranging from arthralgia to severe neurological disability and is caused by either evolved or escaped gas released into the bloodstream as a result of changes in the ambient pressure. Patients can self-refer to DDRC via the British Hyperbaric Association helpline, they are also often referred in by emergency departments and diving centres if they prevent there first. Treatment consists of emergency recompression whilst breathing an FiO2 of 100% to recompress bubbles and oxygenate tissue rendered ischaemic by bubble emboli. If recompression is achieved soon enough after onset, then patients can often achieve complete resolution of their symptoms. DDRC is one of just ten centres in the UK approved to provide this emergency treatment. In addition to this clinical side, DDRC provide many different professional training courses. This includes first aid courses for commercial divers and offshore workers, training on the use of hyperbaric chambers, and the Diving Medical Advisory Committee (DMAC) courses for doctors. The DMAC course 1 and 2 are for doctors with an interest or who wish to specialise in diving medicine and qualifies them to provide both commercial and diving medical certificates or to go on and work as a diving doctor. The courses, which I was fortunate enough to observe, covered a mix of clinical science and practical management of diving related medical conditions as well as insight into the practical aspects of recreational and commercial diving. It was attended by a broad representation of doctors including occupational medical consultants, doctors working at hyperbaric chambers, and military doctors from several different countries. Overall this was a fantastic experience which exposed me to a whole new aspect of medicine which I never would come across within my clinical placements at medical school. Applying medicine to the context of diving enabled me to develop my lateral thinking and problem-solving skills in addition to forcing me to consider common pathologies in a very different way. For anyone interested in learning more about diving and hyperbaric medicine I would recommend the following: • DDRC
https://www.ddrc.org/ All hyperlinks correct as of 29/03/2023.
Matthew Hegarty click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Elective Report- Albania, April-June, 2022
I would like to start by thanking Kidderminster Medical Society for their generous support of my elective to Albania. In the middle of April, I landed in Tirana, Albania for the start of my elective. The hospital was easily identifiable by the streams of people in jeans, t-shirts and white coats heading in one direction. We started our placement in the endocrinology ward. There were around 15 doctors and each doctor specially cared for 2-4 patients. The patients had very ‘textbook’ endocrine pathologies, due to the longer time to seek specialist care- we saw large goitres, grave’s eye disease and acromegaly within the first week, which I had never seen in person in Oxford. Due to the language barrier, we largely observed, with the doctors translating histories for us, and asking the patient’s permission for us to examine. A doctor explained the process to becoming a resident doctor in Tirana, which incredibly involved working without pay for several years, so as to avoid being sent to a smaller town. Many doctors are support solely by family members, though senior doctors also worked in private hospitals. They also explained the differences in patient culture in Albania. Patients in hospital were largely cared for by family members, who were constantly on the ward, with food and supplies, and apparently during the pandemic, many preferred to hire an oxygen tank and treat relatives at home than bring them to hospital. Additionally, due to the large population working abroad, family members brought medicines which were unavailable in Albania back from Turkey and Italy, such as continuous glucose monitoring systems. While on endocrinology we also visited an outpatient clinic, where patients had travelled from all across the north of the country. The appointments were very short and were permeated by interruptions form other patients who waited in a crowd by the door, occasionally entering the clinic room to check if the previous appointment was over, before being sent away by an authoritative nurse. When we asked about this, the doctor laughed and said they and tried to implement a waiting room and timing system, but it had been abandoned quickly as the patients ignored it. Later, we moved to paediatric ICU. The block was brand new, as the previous building had become structurally unsafe following the earthquake in 2019. For such a large block, there were very few children. Despite the polished wards, and incubators emblazoned with sponsorship logos, it was clear some supplies were in short supply. Vials were kept if they were half used, to avoid waste. There were some very heart-warming stories, such as a child who had been born with undiagnosed gastroschisis. This was treated with an operation in our first week, they were out of the incubator in our second week, and home in our third week. It was a complex operation, which may not have been possible until recently in Albania thanks to the rapidly advancing medical system. It made us smile that the nurses gave the family the medication to take home in a fake Louis Vuitton plastic bag, which seemed to be the bag of choice in Tirana. We also regularly visited a charity for children with Down’s Syndrome in Tirana, which had been set up by a mother. They provided free, high quality physiotherapy, speech, occupational and music therapy for children, which was highly sought after, as the state funding for families with disabled children was insubstantial to pay for expensive private treatment. The techniques we saw being used were very up to date, and it was interesting to see how they encouraged integration of the children and young people, teaching them how to work in cafes and shops and in their on-site coffee room. They told us how Albanian society is gradually becoming more accepting of people with Down’s Syndrome, but that there was still prejudice to overcome. In the second half of the elective, we went to a hospital in Saranda, which is in the south of the country, on the coast. Here we were mostly in the emergency room, and also visited surgery. The ED had a similar list of complaints to in the UK- minor injuries, chest pain, chest infections and D&V. Surgery was quite different as they did not have laparoscopic equipment and so appendectomies and other small operations were done as open. They also had reusable gowns and drapes. There seemed to be a more traditional ‘surgeon’ role – it seemed surgery was still very male dominated. Overall, my elective to Albania was incredibly informative both from a medical and cultural perspective. Albania is a country which has few visitors and so we were always treated very warmly by people keen to show off how beautiful their country was. We hope to encourage more students to do electives in Albania and hope to help set up an exchange programme for medical students.
Imogen Jury click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Dear Dr Martin Lewis and the Trustees
To the Trustees of Kidderminster Medical Society
I am writing to convey my gratitude for the opportunity and support provided by the Graduate Entry Medicine Kidderminster Medical Society Bursary during my preclinical year at the University of Birmingham. This bursary has been invaluable during these hard times, where the Covid-19 pandemic continues and the cost of living rises steeply. My first year has been an incredible experience, filled with challenges and many moments of motivating reward. I have benefited from exemplary teaching and a wide variety of informative experiences during my first year of study, all of which I have been able to apply my maximal attention and energy to thanks to the Kidderminster grant.
The bursary from the Kidderminster Medical Society has meant that as a Graduate Medical student, returning to education after 2+ years away, I could reduce my working hours and take more time to focus on my studies. Reflecting upon this now, I realise even more so how valuable the support from the bursary has been. I spent most days, nights and weekends at the library learning the preclinical medical content (2 years in 1), this left me with restricted spare time to work and volunteer, without the Kidderminster grant I would have had to have worked more hours which would have impacted on my learning.
Prior to studying Medicine, I studied Biology. During my degree, I worked part time as a Health Care Assistant and it was during my experiences working in care that I first explored the possibility of becoming a Doctor. I found it rewarding and meaningful to have a role in supporting patients’ recovery and being able to put some of theory of what was learnt during my Biology degree into practice. Following my degree, I began volunteering at the hospital and arranged work experience with Doctors, I also worked as a Research Assistant within the NHS. During the peak of the pandemic I was working in A&E and on the Covid-19 wards, this was a particularly challenging, but also highly rewarding time to be a frontline healthcare worker. Returning to studying after 2+ years out, was undoubtedly a challenge. I had to confront the vast extent of the theoretical content that I was required to learn, but as time went on, and I could dedicate more time to my studies following the bursary award, I grew more confident in my degree and felt better equipped to handle the challenges of the course.
The highlights of my first year have been my Community Based Medicine (CBM) placements, which began online as Covid-19 cases were high but transitioned to being in person at the GP surgeries. The tutor I was allocated for my placement went above and beyond to educate my CBM group, providing us with diverse and enriching learning opportunities. These included shadowing patient consultations and learning from many other doctors, nurses, healthcare professionals and patient experiences. For example, I gained an insight into the lives of different patients living with chronic conditions whilst also attaining a unique perspective of their healthcare journey and the range of services that could be beneficial for treatment. Another highlight of my experiences was learning anatomy and medical imaging analyses from a General Surgeon, whose depth of real world experience was an invaluable resource.
My first year has been full of fulfilling experiences, and this would not have been possible without the support of the Kidderminster Medical Society. I would like to thank you all sincerely for the support you have given to me and other medical students. There is currently a movement amongst medical students, A Liveable NHS Bursary. This movement highlights the limitations of the NHS Bursary and Student Finance England loans available for medical students, meaning that the generosity and support from organisations such as Kidderminster Medical Society truly are some of the only means by which students, including myself, can afford to continue studying Medicine. The Kidderminster bursary has provided me with a safety net for these coming years, and for this I will be eternally grateful. Your support has allowed me to feel excited and eager to continue studies as I enter into my third year at the end of August.
Thank you wholeheartedly for your altruism. Sincerely, Emma Porter click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Dear Dr Martin Lewis and the Kidderminster Medical Society
I would like to begin by extending my gratitude for the awarded bursary. Starting medical school as a mature student is a big leap especially when moving to a new city and dedicating your time to studying once again. Thanks to the bursary I was able to commit fully to my course and partake in the many opportunities available at the university without any financial worries.
First year of medical school has been a challenge but incredibly rewarding. My pre-clinical course has a more traditional approach with lectures, small group teachings, lab-based activities and weekly dissection sessions with our generous donor whom we spent all year with exploring the complexity of the human body. As this is an accelerated course the Cambridge term is very short and packed thoroughly to keep you busy with pre-clinical content. During everyone’s holidays we would head out to our hospital and GP placements for a much-needed break from the academia to gain very valuable clinical experience. Luckily, we were able to spend time with patients and clinicians face to face despite COVID and this challenged us to put what we learnt into practice. My highlights were taking bloods for the first time and practicing my cardiovascular, respiratory and abdominal examinations on patients.
I would not have been able to do this without your help as it allowed me to support myself and as a result use my spare time to immerse myself into not only studying but getting involved in college activities and soaking in the scenic views here at Cambridge. I look forwards to working just as hard during second year to hopefully shape me into a more competent and compassionate doctor in the future. Once again thank you Kidderminster Medical Society for your kindness and giving me a fantastic first year at the graduate medical course.
Best wishes Bahishta Sidiqi
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Firstly, may I start by saying a big thank you to Kidderminster Medical Society for their generous bursary which allowed me to undertake a very special elective placement during March 2022. Given the pandemic, it was a difficult time to be planning an elective placement abroad with such uncertainty about whether the number of Covid cases and entry requirements would allow. However, I finally managed to secure a placement in Bahrain.
This was my first time visiting the Middle East and Bahrain was certainly an amazing experience with its unusual landscape and contradictions resulting from the combination of modern Arabic culture with the archaeological legacy of five thousand years of civilisation. My time was split between King Hamad University Hospital (KHUH) and Royal College of Surgeons Ireland University (RCSI). At KHUH I was assigned to an Endocrinology team with my clinical supervisor being a Professor in Endocrinology. I observed and undertook endocrinology clinics with senior supervision and general medical ward rounds. Additionally, I assisted with all patient care, undertaking clinical skills and patient assessments including reviewing outlier patients and clerking new patients presenting to A+E enabling me to continue to develop clinical and communication skills and improve my confidence for starting my first F1 job in August. Presenting patient cases during daily ward rounds and MDTs also helped to develop my skills in referring patients to seniors- a common job for an F1. Within RCSI, I participated in small-group tutorials on topics such as electrolytes, ABG interpretation and diabetes and was also fortunate to be able to participate in obstetric PPH and normal labour simulation sessions which I particularly enjoyed. I also had the opportunity to deliver group teaching sessions to younger year medical students, enabling me to practise skills I had learnt during my Medical Education intercalated degree. The placement has highlighted differences from medicine in the UK. On a population level, there is a high level of sedentary lifestyles in Bahrain, with high carbohydrate and sugar diets and low levels of exercise. This is a major contributing factor to 15% of the population having Diabetes Mellitus, which when compared to the UK is nearly double (Ministry of Health 2022). There is very strict adherence to separate gender wards complying with cultural practises. Due to availability of resources and population demand for services, endocrine clinics are not split into sub-specialities as they are in the UK, meaning general endocrine, paediatric, gestational and Type 1 and 2 diabetic patients are seen within the same clinic. Bahrain has a Universal health care system with Government provided healthcare being free to Bahrani citizens, but most hospitals appear to be private and paid for via insurance policies, along with prescriptions which also must be paid for, a major difference to healthcare in Wales. In addition, there is no General Practice service in Bahrain; instead, they have local health centres providing care by general physicians and can be accessed by any individual if they have the means to afford it. My placement provided valuable experience of healthcare in different social and clinical settings. I was exposed to different ways of working which was challenging but very exciting and rewarding. I have improved my confidence with basic ward jobs, presenting clinical cases and consolidating medical knowledge. I quickly felt part of the team and my skills were appreciated by my clinical lead. In addition, I was excited to able to share my own experiences such as case-based-learning, (currently being introduced into the Bahrain medical curriculum) and to discuss the advantages of new concepts such as SOCRATES, defined roles during simulation sessions and structure of case presentations. This placement provided a very positive and rewarding experience, and confirmed that I can be independent, which in turn improved my confidence working in new, unfamiliar situations, something I will continuously be exposed to as a doctor. The language barrier was sometimes a challenge whilst on the wards, with patients often having very limited English, but I was well supported by the clinical staff and even attempted to speak the little Arabic I have learnt. I was provided with exposure to many different medical wards, clinics, and clinical experiences and was able to also visit one of the military hospitals to see a different style of healthcare/services, widening my understanding of the whole healthcare system. I thoroughly enjoyed my experience, immersing myself in a different culture- trying local food, visiting places of worship, and as I said, learning some basic Arabic. This was the first time KHUH and RCSI have taken an overseas elective student and due to its success, they now intend to set up a more formal programme offering set elective placements in the future. However, with the pristine wards, luxury clinic areas and limited waiting times this all must come at a price, and we should in the UK be forever grateful for the free if not overstretched NHS!
With grateful thanks Olivia Crannage click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Dear Dr Martin Lewis and the trustees of the Kidderminster Medical Society,
Starting medical school in September, was like no other year in history. With online classes, lockdowns, and a global pandemic it was an extraordinary experience. However, despite all of this I have still had an incredible first year at Warwick Medical School. None of this would have been possible without Kidderminster Medical Society to whom I would like to wholeheartedly thank. The support I received from the Graduate Entry Medicine Bursary enabled me to totally focus on my studies and not have to worry about my financial situation. First year was challenging, the amount of information covered was absolutely staggering, especially being out of education for a few years, I found that I really had to go back to basics. Despite this, the teaching was fantastic, the highlight of my year being Fridays as this was the only day, I was in the medical school to learn anatomy and clinical skills. Other highlights of the year included case-based learning (CBL) in which groups of 8 students work through a clinical scenario together. This has been a really great experience, allowing me to learn so much from my fellow students, who due to their various backgrounds bring so much knowledge and experience to the group. Additionally, I really enjoyed community days despite not being able to visit patients in person, it was still a fantastic opportunity to talk to patients over the phone and learn more about their story and experiences. I am really excited for second year and what the future brings. I am committed to my education and one step closer to becoming a doctor thanks to your generosity and support. I will forever be thankful for this.
Yours truly, Beth Stinchcombe click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
I would like to thank the Kidderminster Medical Society for their generosity in awarding me the Graduate Entry Medicine Bursary. This bursary has been a significant source of support during a period of such uncertainty and has made my return to education after four years in employment feel less overwhelming. The bursary has enabled me to immerse myself into my studies and successfully make the jump from humanities to science. Studying medicine from home is a daunting prospect, especially when in your first year. At first, it was a rather lonely experience, but as time went on the rhythm and dynamics of online lectures and group work sessions became second nature and I took the impact of the developing pandemic on my education in my stride. The brilliant efforts of Leicester Medical School ensured that we still received an excellent and thorough education. When life and education regained some semblance of normality, we were able to visit the Dissection Department which was a major highlight of the year for me. For the first time, we were able to see all the different organs that we had learnt about in books and lectures for the last year and how they lie comparative to one another. This was certainly a very rewarding ‘light bulb’ moment in my learning. Another highlight which came with the easing of the pandemic was our Healthcare Assistant training. For many of us, this was our first time on a ward with patients. I was placed on an elderly care ward which specialised in Dementia. The complex and varying needs of the patients I spent time with made me appreciate the vital importance of holistic care. I realised that tending to the psychological and social as well as physiological needs of a patient is paramount to a quicker and stronger recovery. Additionally, I also gained an appreciation for teamwork and the integral parts all health workers play across the NHS in delivering optimum patient care. Being able to finally spend time with patients was a great way to end the academic year because after many months of studying from home, it served as a reminder for why we are on the course and how immensely rewarding the world of medicine is. I attribute my brilliant first year of medicine to this bursary because it has enabled me to embrace every learning opportunity which has come my way. Kidderminster Medical Society has certainly stood me in good stead for the next 4 years, for which I will be evermore grateful.
Kind Regards Helen Field click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Dear team at the Kidderminster Medical Society,
Thank you ever so much for your extremely generous bursary for the 2020/21 academic year. As you know, I started graduate entry medicine at the University of Birmingham Medical School in September 2020. This has been an absolutely fantastic year and I have gained an immense amount of knowledge. This has been a very academically challenging year, learning human biology in such a short space of time! This was particularly difficult with it having been 5 years since graduating from my Biomedical Science undergraduate degree, after which I then completed my PhD. So, returning to formal taught university learning has been challenging! However, despite this I passed all my exams, and I cannot believe how I did it, but I was awarded over 70% in all my overall exams! I am now very excited to proceed into my clinical years from September. Due to how challenging I found the year, I have had very little time to do much work for my research fellow contracts at the University of Birmingham Institute of Cancer and Genomic Sciences and the Medical Research Council Clinical Trial Unit at University College London. This has meant very little time to make any money! – Hence, your bursary has enabled me to live without having to compromise my studies to find the time to do my paid work. COVID-19 meant that the majority of our year was taught and examined online, however, the university organised this extremely well and this did not disrupt our learning. It also enabled me to keep my family safe, not having to spend time on campus. Due to COVID we were not able to be on site for our clinical community general practice days, which meant hands on experiences were more challenging. So, your money enabled me to purchase pieces of equipment to practice with (on my poor family!). I purchased a manual blood pressure monitor and a peak flow device. Your money has also set me up for my clinical years, for example, buying my medicine bible – the Oxford Handbook of Clinical Medicine. I have not had to use money for travelling this year, due to the remote nature of our studies. However, I will be driving a couple of hours every day to get to my placement hospitals and your money will considerably help towards my fuel, and I am sure hospital parking! I am so lucky to have many connections with the Worcestershire area, including spending much of my time living in the area and commuting to university from there. I am hoping to be placed at a Worcestershire hospital at some point during my studies. I continue to enjoy road biking and running through the Wyre Forest area. My bursary has also enabled me to purchase a race slot at my first Duathlon (Run 10km-Bike 44km-Run 5km) event, which I am currently training for (thank you to the Wyre forest area for providing me with plenty of hills to train on!). Once again, thank you ever so much for your very generous help, I will keep in touch,
Hattie (Harriet) Mintz BSc PhD click to go to Index at top of page
Dr Hattie (Harriet) P Mintz BSc PhD
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Thank you letter from Stuart Evans (2017)
Hi Martin I just wanted to let you know that I received my examination results for my finals examinations on Thursday. I am very pleased to say that I have successful completed medical school with a distinction in every exam (except one, where I slipped to a merit!) I would just like to thank you again for the bursary you provided to me at the start of my degree, it certainly made the financial burden a little easier! I hope you are well and COVID hasn’t caused too many problems. Best Wishes
Dr Stuart Evans BSc (Hons), MBChB, PG. Dip
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Bursary Report from Bryony Garfield Wow – what an unexpected end to a first year of studying at Warwick Medical School! Thank you to all at Kidderminster Medical Society for the Graduate Entry Medicine Bursary. The bursary enabled me to fully throw myself into each and every learning opportunity without having to think about the financial consequences as much as I would have done before the bursary. I really have appreciated this and it has enabled me to say “yes” to more extracurricular activities, such as doing Basic Life Support training in the evenings, which will hopefully help in the future as a Doctor.
A particular highlight of the year, aside from seeing beautiful specimens in the anatomy labs on Fridays, was visiting patients in community to see how they cope with their chronic and sometimes rare conditions. Speaking to the patients, carers and a variety of healthcare professionals has really opened my eyes to how important it is that we all work together to help improve the patient’s quality of life. It has also highlighted a need to focus on what the patient is telling me, especially with rarer diseases, as they are likely to know a lot more about their conditions than I will as a junior. Communication is so imperative, and I am incredibly grateful that I could spend the time chatting to and learning from people before the pandemic took over the degree.
With the changes to academics caused by the pandemic, I was able to focus on my studies during the lockdown without having to try and fit a part time job alongside this. This was largely due to the support from the bursary and I am truly appreciative of this. Thank you all once again and I truly hope that 2021 is less eventful for all. Bryony Garfield click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Graduate Entry Medicine Bursary Report – Will Hodgeman
Firstly, I would like to extend a huge thank you to Kidderminster Medical Society for the opportunity and support provided by the Graduate Entry Medicine Bursary during my first year at The University of Glasgow. It has been an incredible help over the past year, especially in such an unpredictable time. My decision to return to university life after a previous degree and year away has unsurprisingly presented some unique challenges, and the support of this bursary has allowed me to combat those and ensured I have made the most of the past year.
Despite a somewhat strange ending to the academic year I have thoroughly enjoyed my first year on the Medicine course. The structure and focus of the course has assured me of my resolve to continue my studies and career in Medicine and I am excited to see what the future has to hold. The last couple of months of the academic year were extremely unpredictable, with the medical school doing all they could to ensure we were still provided with all the necessary learning and examination experience. The support of the bursary allowed me to focus on this improvised and altered teaching structure without having to worry about my living or working situation alongside the inevitable stresses of studying. Furthermore, over the past year I have been able to supplement my day to day studies with extra-curricular and social medical events, due to the support and financial stability provided by this bursary.
Over summer I have been able to undertake a small remote research project assisting a cancer research laboratory at Texas A&M University College of Medicine in the writing of a review paper. This has been extremely valuable to my studies, with the focus of the review covering large aspects of my first-year studies in immunology, epigenetics, and gastroenterology, and a solid basis to topics yet to be covered on the course. It is also a fantastic contact to have in a superb medical facility. This opportunity was facilitated by the bursary, allowing me to focus on this project over summer rather than work. Indeed, this demonstrates how this bursary has not only supported me and provided valuable opportunities over the past year, but that its impacts will continue to be seen throughout my studies and beyond.
Many thanks for all the support, Will Hodgeman
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Bursary Report from Jamie Richardson I would like to express my appreciation to the Kidderminster Medical Society for awarding me the 2019/2020 bursary. It is such a generous amount of money and it has greatly helped me throughout my first year studying graduate entry medicine at the University of Birmingham. At the start of the year I had planned to work at the weekends to help fund the first year of my degree. However, thanks to the Kidderminster bursary I did not have to do this. Not having to work at the weekends allowed me to keep on top of my studies throughout an intense year. Moreover, not having the pressure of working at the weekends allowed me to pursue my passion of playing football; I played for the medical school football team throughout the year. GEC1 has been an intense year, however I have thoroughly enjoyed it and I have learnt so much. The first year of my studies has largely been based on problem-based learning (PBL). When learning in PBL we would work in groups of around 8 students, this has been very enjoyable and has enabled me to make friends with people on my course. The highlight of my first year studying medicine has been my community-based placement. I have relished having the opportunity to interact with patients and to learn clinical skills. I have found it fascinating meeting with patients to take their medical history in order to try and understand their presenting complaint. The Kidderminster bursary has not only helped me to fund the cost of commuting into University but also the cost of commuting into my community-based placement. I am very much looking forward to starting GEC2 and I am taking steps to ensure that I am fully prepared to start my clinical placement in September. Once again, I would like to thank the Kidderminster Medical Society for awarding me the bursary it really has made a huge difference to my first year at Birmingham.
Once Again, Thank You Jamie Richardson
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||
 |
||||||||||||||||||||||||||||||||||||||||||||||
|
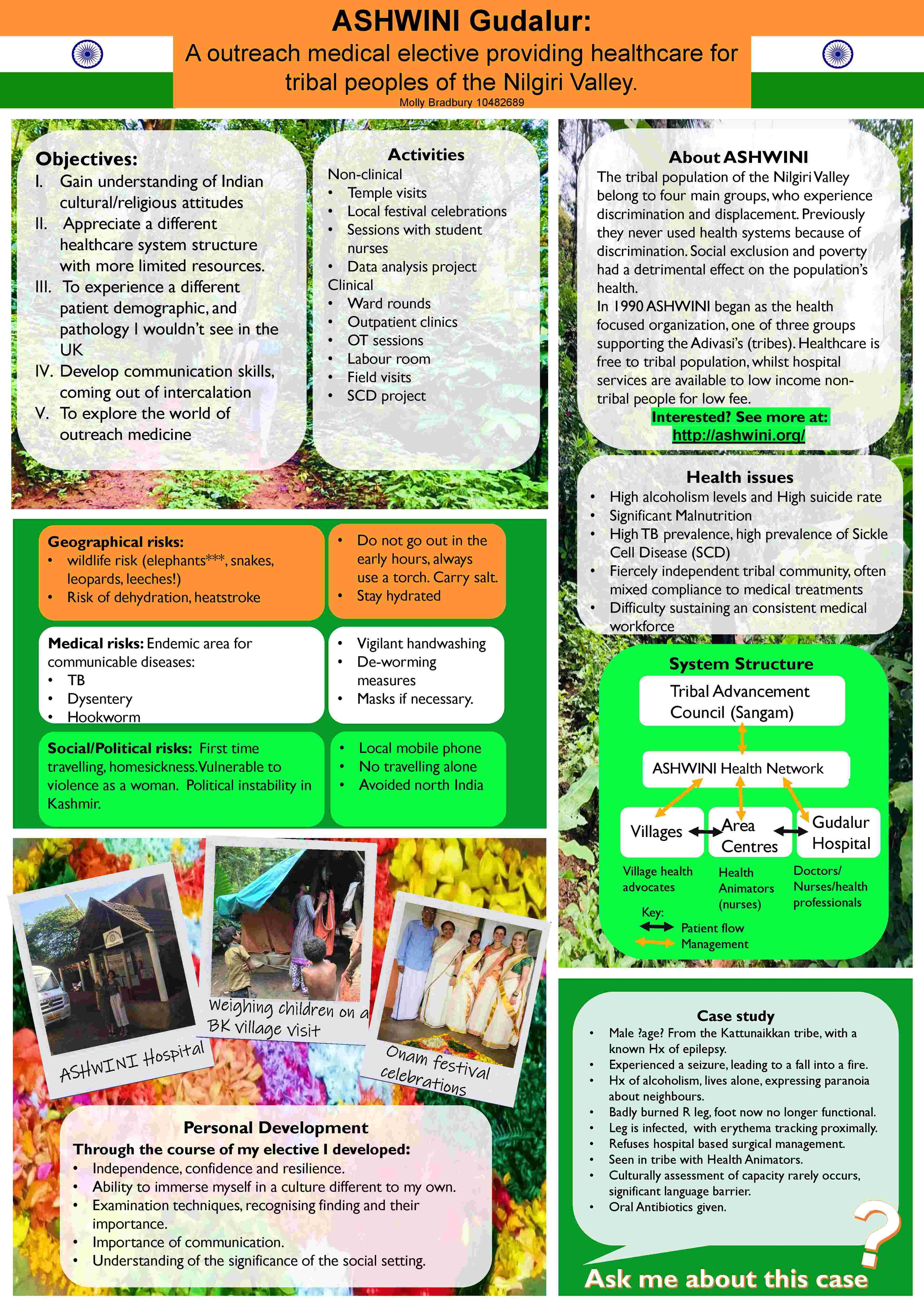
Sent on behalf of Dr Sarah Ford Dear Molly, Thank you for submitting an excellent poster and outstanding presentation which have combined to reflect an elective experience from which you have clearly benefitted both professionally and personally. This year, the standard was truly excellent as there have been three students who have been awarded the highest possible score. The prize money will therefore be shared so that you will all have this accolade on your CVs. I would like to congratulate you on this achievement on behalf of the elective advisors. The prize has to be confirmed by the Award Board and the prizes and awards team will be in touch with you regarding the presentation of the award. Best wishes, Sarah Ford,
Molly Bradbury |
||||||||||||||||||||||||||||||||||||||||||||||
|
Final Elective Report from Kim Esquivel
Reflective summary
The organisation of ICU in Bach
Mai Hospital During my elective placement, I spent 3 weeks in the Intensive care unit (ICU), where I was able to shadow Consultants on their ward round and have bedside teaching where we discuss each case on the round. The ward round involved daily investigations to monitor the progress of each patient whilst altering the management plan accordingly. The ward round consists of medical students and doctors, where 2 consultants was in charge for one half of the patients in ICU. After the ward round, both doctors would have a daily handover with nursing staff so that they are both fully aware of each patient case regardless if they are in their delegated half. The roles of the team were different to my clinical experience in the UK because apart from nursing staff and doctors, there was a limited variety of healthcare professionals. For example, I expected to see an ICU ward with specialised physiotherapist to aid patients in their long term stay in ICU. However, it was the nurse’s role to perform physiotherapy to mobilise patients if possible and perform respiratory physiotherapy to remove secretions. In this situation, I felt that by having nurses’ conduct a physiotherapy, it reduced the amount of healthcare professionals looking after the patient and patients would form a stronger relationship with their nursing staff as it was one to one care. However, the nursing staff may be more stressed with an increased workload.
Management of patients in ICU Many of the patients in ICU had a hospital stay in average of 40 days. I found this very unusual as most patients in critical care in the UK would only have 7% of patients stay longer than 11 days. The main trouble was that new patients requiring ICU beds were often dealt with in normal wards as there would be no beds available in ICU. I think that this is a common problem in both east and west with bed management, as the need for healthcare services increases but the availability to provide services remain static. Patients would become frustrated with the doctors, and in Vietnam, the family members would stay in the waiting lounge with their sick family member until they can get a bed in ICU. This increases the strain in the doctor-patient relationship as patients get frustrated, doctors feel inadequate as they can not provide the care without extra hospital space. The problem in ICU is that long-term patients would usually be very complex, and doctors are often at a loose end with their management plan. In Vietnam, palliative care has not really been established. Doctors would have discussions with the family members of an unconscious comatose patients in ICU, and although they say the prognosis is dire, the family would still wish to carry on life sustaining treatment. Often the family would pay extra to keep the patient in their ICU bed and maintain life sustaining treatment. On the ward there was a patient who has suffered a myocardial infarction and required stenting to re-open the coronary vessels. Whilst most patients post stenting would be allocated to a bed in the cardiology ward, this patient had special treatment due to the family’s wealth.
The consultant in
charge disclosed that because this patient’s
family is paying extra, they have allocated the
patient an ICU bed for more close monitoring due
to family wishes.
This case is not uncommon in Vietnam and studies have shown that monetary gain can equate to better treatment in hospitals. However, with regard to the doctor-patient relationship, the doctor may feel that their judgement is undermined by the patient or the family members because they have paid for the medical decision. The best interest for the patient may not necessarily correlate with the family members decision but with money involved the doctor may feel pressured to cave to the family’s wishes. I think that this behaviour is detrimental to the doctor-patient relationship, as family members would not know the best medical management for the patient and it is the doctors job to communicate effectively what they believe should be the next step. The culture in Vietnam with regard to preserving patient’s dignity and comfort during examinations was very different from my experience in Medical school. I found that patients during ward rounds would usually be unconscious or have a low consciousness level due to the severity of their disease in ICU. All of the bays on the ward did not have curtains for privacy and many patients would have no gown on the upper body so their chest would be exposed to other patients and members of staff. I found this uncomfortable to see, as we are always told in Medical school to maintain patient’s dignity during physical examinations. I felt that doctors should have made the comfort of the patient a priority, as they were too unconscious to object to the insufficient care provided. Walking past other wards in hospital I found that procedures were being done in front of families such as catheterisations, with no curtains to preserve the patient’s privacy. I was shocked to see this when moving from ward to ward. This showed me the importance of the family members role in the doctor-patient relationship. In Vietnam, the family members would be given equal or more priority than the patient when it came to making decisions. The impact between the doctor-patient relationship means that the decision would often lie between the doctor and family member, as the patient would be to ill to advocate for themselves. This situation has taught me that as Doctors we should always advocate for the best interest of our patients and have the confidence to make our point across to family members, as stated in the medical ethics of beneficence.
My experience in
Obstetrics and Gynaecology
For the last 3 days of placement, my rotation was in Obstetrics and Gynaecology. During our clinical years, we have not had any experience of this specialty previously. My daily activities involved observing in outpatient clinics, ward rounds and theatre lists. The structure of the department was interesting as it encompassed everything in one ward: from outpatient clinics for antenatal scans, to the labour room and post delivery suite. The theatres for caesarean sections was located in the floor above with a post-surgery maternity ward. In the outpatient clinics, women would come for their antenatal scans and be surrounded by 15 medical students, the doctor and one ultrasound machine. As a patient, I would have felt very intimidated in this situation, as a crowd of people were observing my scans. Fortunately, most women were unfazed, however most clinics in the UK would have a maximum of 2 students to preserve patients’ privacy. I think that in this situation the medical student’s education was prioritised, and it could be improved if the doctors asked for consent to having only a few medical students during the clinic. By having a crowd of people in the clinic, this would have been a barrier between the doctor and patient communication as it would have felt quite impersonal. Therefore, if the patient wanted to disclose any personal concerns or if the doctor had to break bad news, it would have been very difficult to form rapport with a large group of observants watching the consultation. The labour room could occupy 10-20 patients, whereby patients would not be separated by curtains, therefore during intimate examinations the patient would be overtly exposed. Being taught that the patient’s dignity should come first before any examination, I found this quite shocking as other patients could see the intimate examinations taking place. I felt that in this situation, the patient was in excruciating pain to have the strength to contest the doctor in conducting an intimate examination in front of others. Most women in the labour room were all nearly fully dilated before being taken into the delivery suite which is mainly midwife-led with an overlooking doctor on duty. In the labour room, the women would not be given any painkillers such as Entonox, epidurals, pethidine or even having the choice of being in a birthing pool. This has taught me to value the luxury of medications in the UK, and value a healthcare system where our comfort is made a priority. Many thanks Kim Esquivel
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Bursary Report from Bethany Davies
Firstly, I would like to thank the Kidderminster Medical Society for their contribution to my elective this year. It helped fund the trip of a lifetime to the Princess of Wales Hospital in Sydney, Australia. I was based in the Oncology Department in the suburb of Randwick-located hospital just outside of the big city. I was anxious about visiting a place so far away alone however I soon settled in. I soon became to realise that while there were many differences between the UK and Australia, there were also several similarities. One of the similarities was the level with which the hospital treated patients at. By this I mean, it was very much a ‘developed country’ hospital – with up to date technology, various highly trained and specialised departments with cutting-edge treatments and clinical trials. My day to day schedule was also familiar to me – sitting and participating in different oncology clinics with a consultant, attending multi-disciplinary team meetings and joining ward rounds. Other activities I took part in included observing radiotherapy-planning sessions, going on home visits and attending genetic counselling. However, there were particular days that stood out to me. One such day was when I was placed with the palliative care team and we conducted home visits. We attended a lady with advanced multiple sclerosis who was only in her 40s. Her husband and young children could only just understand how she spoke and she could no longer eat solid foods. It was extremely moving to see the family dynamics and to hear about her rapid decline of a year. The team organised adjustments to their house, for carers to come in and, of course, the medical side of helping with breathing and eating. This experience touched me and allowed me to appreciate what I have but also understand how palliative care can truly help someone and their families. Another day that stood out to me was seeing someone get told they have stage 4 cancer for the first time. It was a gentleman in his 60s, and his wife and 3 children had all come to the appointment to support him. He had an idea that it was a serious diagnosis but did not understand the gravity of the situation. When he and his family broke down upon hearing the news I could not help myself welling up. I observed tremendous communication skills from the doctor who displayed empathy and humility alongside professionalism and control. Whilst being extremely upset, the family left with a plan and the support they needed at this distressing time, which was invaluable. This is definitely something I will take forward in my future career. A final day I remember is attending genetic counselling sessions. I was fascinated with how the diagnosis of one can affect so many. I understood the concept before but had never seen it ‘in action’. A woman had been diagnosed with Li-Fraumeni syndrome, an autosomal dominant disorder caused by a mutation in the p53 gene. I had never seen anyone with the condition let alone appreciated the effect it can have on their wider families. The consultation consisted of going over her diagnosis (she had had breast cancer a few years ago and just had a sarcoma removed), and then discussing any ongoing treatment and wider implications. A family tree was made and she gave consent for her family members to be contacted for genetic testing. It was interesting to see genetic counselling in ‘real life’ and the importance of helping the patient with their troubling diagnosis, maintaining confidentiality, whilst also considering other family members. I also appreciated how Australia have their version of NICE that contains their recommended treatments. However, how people access this medical treatment over there is different due to the dissimilarities in funding – private or public. You can pay for private medical insurance or be a part of the government funded Medicare system. In the UK, money does not even get mentioned in any public healthcare setting. However, in Australia, funding is at the forefront of conversations, even just to ask to see their Medicare card on reception. There were also multiple forms to fill out and coding systems to ensure the correct money was billed to the right place. It definitely made me appreciate our National Health Service and how it should be protected. In conclusion, I cannot thank the society enough for contributing to this trip. It gave me the chance to see how healthcare can differ in another well-developed country, but, also highlighted the similarities of how we all strive for the same thing. The experiences I encountered will help me be a better doctor both in terms of knowledge and non-technical skills. I would definitely recommend the beautiful Australia as an elective destination and I look forward to starting my career this August.
Best Wishes and Thank you Bethany Davies
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Bursary Report and Elective – Hayley Slater Site of Elective: Trauma Department Chris Hani Baragwanath Academic Hospital, Johannesburg, South Africa
Introduction: Chris Hani Baragwanath Academic Hospital is the third largest hospital in the world and the largest acute hospital. It is located in South-West Johannesburg and serves more than 5 million people. Many of the patients come from Soweto – A township of approximately 3.5 Million people and one of Johannesburg’s poorest townships. (1) The Chris Hani Baragwanath Hospital occupies around 173 acres (0.70 km2), with 3,200 beds and 6,760 staff members. The facilities are housed in 429 buildings with a total surface area of 233'795 m2. 70% of all admissions are emergencies, including 160 victims of gunshot wounds per month. South Africa is regarded as a leading authority on trauma medicine and surgery, primarily due to the high rates of trauma admissions. South Africa has a noticably high rate of murders, assaults, rapes and other violent crimes compared to most countries (2). Over 90% of global trauma deaths occur in Low- and Middle-income countries (3). Recent publications from the World Health Organization place the global injury mortality rate at five million per annum, with almost one-fifth in Africa.(3) In the near future, the injury mortality rate will exceed that of HIV and AIDS, tuberculosis, malaria and obstetric causes combined. (4) Over 50 000 trauma- related deaths were recorded in 2009 across South Africa, with the majority related to transport and violence. (5 As someone interesting in emergency medicine, I chose trauma in South Africa as a way of gaining exposure to an area of medicine that is seen far less often in the UK. “Casualty” at Chris Hani Baragwanath Academic Hospital know as just “Bara” to the locals is divided into three separate areas; Medical – for all medical issues, Surgical – for surgical emergencies such as acute appendicitis, cholecystitis or renal colic; Patients must be referred by a local clinic to access this department. Finally, Trauma – again patients should be referred from one of the smaller clinics as Bara is a tertiary centre and much of the more minor trauma can be dealt with elsewhere. On arrival patients are “screened” by a senior doctor. This functions as a triage service, although no observations are available. It designates patients as either unstable, stable or unsuitable for Bara. Unstable patients are transferred immediately to the resus department. There are fourteen monitored beds in the department with approximately three nurses, although often only one nurse is fully registered. The department also has a “LODOX” machine. This is a low dose x-ray enabling patients to be scanned within the department upon entry. This allows patients’ larger injuries to be immediately recognised and managed early. The resolution does not allow for detailed assessment but does identify pneumothoraces, long bone fractures and bullet trajectory. Patients are stabilised in the department and then transferred to theatre, trauma ward or trauma ICU. Stable patients are sent to the admin department to book in; this is where patients are registered, and payment is arranged. Payment amounts are based on income. Most patients have very low or no declared income. Once registered the patients can return to the department to be seen. They may then be sent for x-rays or other investigations, reviewed by senior doctors and either discharged or admitted. A lot of these patients are referred to orthopedics who are not based in the trauma department. All patients have to be cleared by trauma before they can be referred. Outcomes of Intended Learning Objectives Major trauma is managed expertly in South Africa if Chris Hani Baragwanath is representative; as one would expect from a country that experiences so much trauma on a daily basis. The average week in resus saw at least 100 cases. These were divided into penetrating (shooting and stabbing), blunt trauma (vehicle accidents and mob assaults) and burns. I was able to be involved in many of these – especially during the course of the 24-hour shift. My interest was primarily in the stabilization, initial investigations and management of these patients and I got a good understanding of the general system employed. In particular the use of sedation, intubation, fluid resuscitation and initial management such as burn scrubbing, pressure dressing and skin traction. Overall, I felt that I achieved this objective. As expected, the vast numbers of trauma patients meant I was able to assist in a lot of cases. In fact, unlike at home, students are a vital part of the workforce. On many occasions I was the only assistant to one senior doctor expected to do everything required. I was then often left to complete primary management alone, while I was initially apprehensive about this, I came to enjoy the responsibility and it allowed me to develop my skills at a much faster rate. Generally senior doctors were available if I was unsure or didn’t know how to proceed but there was an expectation that more basic tasks would be done unsupervised. Finally, Bara is well equipped compared to many of the more rural hospitals in south Africa; as a result I don’t think it would be fair to claim that I know how trauma is managed throughout the country but Bara is the undisputed centre for trauma and many protocols were developed there. Learning Objective 2: I was able to and in fact, expected to preform many procedures. For basic things like suturing I was able to do daily. I was able to improve my ability and speed. I also had to suture in layers for deep injuries, most memorably a pig bite and in numerous difficult areas such as the scalp, face and hands. Resource limitations also forced me to improve my abilities as well; On one occasion, I had to suture a stab victim using only a large colt needle and hand tying all the sutures as there was no suturing equipment in the department. In the resus department I did many large bore cannulas and blood gases a day which has massively increased my confidence in this area. I was also able to do more advanced procedures under supervision. I inserted a chest drain for a haemothorax and assisted on many central lines. The senior doctors were very keen to teach these procedures and the majority were very patient teachers. After working in such busy departments, they had seen everything and remained unphased in all situations, this helped instill confidence in me. When I ini
Discussion: The volume of patients as well as poor organisation means things take a long time, especially for those that are not unstable. At first, I kept wondering why parents were bringing their children in at 2am with injuries sustained at school – in reality they weren’t but due to the number of different stages and the waiting at each point it was taking several hours until they were properly assessed. The nurses were, like many were underpaid, underappreciated and over worked. However, many were also living in the poverty and violence of Soweto. Many of the nurses were not fully trained. Most traditional nursing tasks were performed by medical/elective students. I got used to being ignored by nurses and having to repeat requests several times. After several days I started to appreciate that this wasn’t personal but rather a reflection on the system. I got used to being more demanding and repeating requests. Often this was for analgesia, I’m not used to working a system that requires multiple requests to get something so basic; especially for patients who in many cases had very serious injuries. Patients themselves are often completely ignored by the nurses so I had to advocate on their behalf. I hope to take this advocacy back to the UK, as well as an even greater appreciation of our very dedicated and caring nurses. Financial limitations, doctor shortage, exhaustion and an attitude of “you find it broke; you leave it broke – your job is to survive your trauma rotation” means service improvement does not happen easily. Many of the doctors had spotted the easy improvements but the grueling hours and resistance from nursing staff meant that after one or two shifts the vast majority of doctors gave up on trying to improve anything or even think about the problems. Surviving the rotation became the priority. The week before I arrived, a gunman (trying to finish what he had started with another man now in trauma resus) managed to get into the department and threaten staff. In another area of South Africa, a junior doctor finished a 40-hour shift and drove home, exhausted they crashed, killing themselves and another driver - the survival they talk of is more than figurative. I worked 24 hours shifts that turn into nearly 30 hours by the time the morning work is completed; The exhaustion is unbelievable. The interns and residents maintain that you get used to it, but I definitely noticed how many mistakes I was making; luckily nothing serious but even simple tasks took much longer. Again, this plays a part in the inefficiency of the system. It is worse for more senior doctors who are making big decisions and preforming more complex tasks with this level of exhaustion. tially struggled with the chest drain, my supervisor was able to encourage me to carry on and ultimately it was successful. Compared to the UK I felt that they were much more comfortable in letting junior member of the team do things even in unstable patients. This is probably a reflection of their own training, in many hospitals a doctor with two years’ experience would be the only doctor available and so skills are expected to be built much quicker as it is often a case of “me or no-one”.
Initially I was completely overwhelmed by the cases I was seeing. I have never seen a gunshot victim before, and I saw six in my first six hours. I had seen one stabbing and within twenty minutes I was suturing stab wounds. I didn’t even know what community justice was but after two days I was able to do the initial management on my own. However, after the initial shock at the types of injuries and sheer amount of cases another feeling was at the forefront of my mind; Why, why is there so much trauma. Six weeks is not enough time to fully understand this incredibly complex nation, but I tried to develop some appreciation. Chris Hani Baragwanath is a microcosm of what is happening in South Africa. The stresses of the broad social, economic and political changes in the country are reflected here. South Africa is the most unequal country in the world; some of the poorest people in the world live in close proximity to people who can afford private education, cars, large houses and staff to clean those houses. Much of the wealth is still focused in the white population as a hangover from apartheid. Both poverty and inequality contribute to the high levels of crime. Attempts to redistribute some of the wealth have also created problems. Corruption is also a massive problem and again could be seen in Bara. I had previous experience of low-resource medicine in Ghana and I believed I was prepared for the limitations I would face in south Africa – I was not. Primarily because in many ways the resources were not limited, at least not in the way I expected. Bara has 4 CT scanners, an MRI machine, the ability to run all urgent blood tests and on one occasion I was even able to witness a trauma patient getting a same-day barium swallow for a suspected oesophageal perforation. There are several trauma theatres in which to perform the many surgeries that take place daily. There is laparoscopic capability. None of this was what envision from resource limited healthcare. However, there were often times when there were no gloves in the department, or normal saline or cannula of the right size. Large parts of several shifts were spent looking for the requisite equipment, which was somewhere in the department, but nobody knew where. This was not the end of the inefficiency; often cheap simple things were not available so more expensive items were used in place. For instance, catheter tubes were often stuck using tegoderm cannula dressings as there was no simple tape. Normal gloves weren’t available so sterile surgical gloves were used for simple examinations. With the numbers of patients this obviously represented massive inefficiency in time and money. I did speak to several of the doctors about this and they pointed towards corruption; the staff purchasing equipment often purchased from friends or family; there was no tender process or transparency. The items therefore were often of poor quality or not available. This is apparently an open secret in South Africa. Overall it was a fantastic experience, I learnt a lot and improved many of my emergency medicine skills however, my biggest take home is how much I appreciate the NHS. The staff, the resources and the organisation.
References: 1. “The Chris Hani Baragwanath Hospital, South Africa | The World’s 3rd Biggest Hospital, in South Africa - Accessed June 7, 2019. https://www.chrishanibaragwanathhospital.co.za/. 2. Matzopoulos, Richard, Megan Prinsloo, Victoria Pillay-van Wyk, Nomonde Gwebushe, Shanaaz Mathews, Lorna J Martin, Ria Laubscher, et al. “Injury-Related Mortality in South Africa: A Retrospective Descriptive Study of Postmortem Investigations.” Bulletin of the World Health Organization 93, no. 5 (May 1, 2015): 303–13. https://doi.org/10.2471/BLT.14.145771 3. Lozano, Rafael, Mohsen Naghavi, Kyle Foreman, Stephen Lim, Kenji Shibuya, Victor Aboyans, Jerry Abraham, et al. “Global and Regional Mortality from 235 Causes of Death for 20 Age Groups in 1990 and 2010: A Systematic Analysis for the Global Burden of Disease Study 2010.” Lancet (London, England) 380, no. 9859 (December 15, 2012): 2095–2128. https://doi.org/10.1016/S0140-6736(12)61728-0. 4. “Crime in South Africa.” In Wikipedia, May 20, 2019. https://en.wikipedia.org/w/index.php?title=Crime_in_South_Africa&oldid=897903898. 5. “WHO | The High Burden of Injuries in South Africa.” WHO. Accessed June 7, 2019. https://www.who.int/bulletin/volumes/85/9/06-037184/en/. 6. Hardcastle, Timothy C, Damian Clarke, George Oosthuizen, and Elizabeth Lutge. “1 5 Trauma, a Preventable Burden of Disease in South Africa: Review of the Evidence, with a Focus on KwaZulu-Natal,” 2016, 12.
Hayley Slater
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Graduate Entry Medicine Bursary Report
I would like to thank the Kidderminster Medical Society immensely for the support that they have given me on the Graduate Entry Medicine Course at University of Birmingham. This has been a year of immense change in my life, where I have taken the leap from a paid job back to university to pursue my ambition of becoming a doctor. The Kidderminster Medical Society bursary has been instrumental in supporting me on this Graduate Entry Medicine Course. This year I have had to adapt again to the lifestyle of a student, and the daunting prospect of supporting myself without a source of income. The first year of the graduate entry medicine course was a challenging and time consuming year. Having just finished, I can now see that undertaking part time work would have been detrimental to my studies. I therefore thank the Kidderminster Medical Society for their support in allowing me to fully concentrate on my studies. With the support of this bursary, I have quickly adapted to the Graduate Entry Medicine course. I have thoroughly enjoyed this first year and the problem based learning environment and I am delighted to have just found out that I have past the first year of this programme. This summer I found some short term work purifying and characterising recombinant surfactant protein D protein in a research laboratory, a protein currently being developed to prevent inflammatory respiratory disease in premature neonates. I have also found some additional work to help write grants and research papers to understand the dysregulation of the immune system in patients with chronic obstructive respiratory disease. I am looking forward to learning in a clinical environment from September. I am excited about my future as a clinical doctor and would like to thank the Kidderminster medical Society for supporting me along this journey. Thank you, Alastair Watson
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Graduate Entry Medicine Report Jeremy Rison
Firstly, I want to express my thanks to the Kidderminster Medical Society for the 2018/19 grant. It is such a generous amount and has been a great help in my first year of Graduate Entry Medicine (GEM) at the University of Nottingham. Not only has the grant eased the financial burden of returning to study and the associated living expenses but it has also covered my travelling costs which have enabled me to keep volunteering with a charity called Birmingham PHAB Camps. We organise and run holidays for disabled and non-disabled children from Birmingham. I have volunteered with this charity for a number of years and being able to continue volunteering with them has been wonderful, as well as providing nice breaks from studying medicine! The first year of studying GEM has been incredibly intense but I have really enjoyed the challenge. It is quite incredible the amount I have learnt this year. Whilst walking into university each morning, I have regularly pinched myself that I am actually studying medicine, something I have wanted to do for many years. I have also made many new friends at medical school and we have helped support each other through this challenging first year of GEM. At Nottingham, we have covered 6 modules in the first year (an introductory module; respiratory; cardiovascular; limbs and back, alimentary; and endocrine). Despite the daunting amount of information we need to commit to memory for exams, I did enjoy bringing the knowledge together at the end of the year. It is difficult for me choose which area of medicine has been my favourite so far as I have found it all so interesting. However, I really enjoyed endocrinology, despite having to revise everything we had covered this year during the module in preparation for summer exams. I also particularly enjoyed my GP placements and the ‘Community Follow-Up’ project where pairs of students have been connected with patients and their families to learn about their use of health and social services. I think this is a great project for medical students as it reminds us of the reasons we chose to study medicine in the first place; something we sometimes need when we spend so much time with our heads down reading and studying. I am currently enjoying a well-earned summer break and am looking forward to completing the last 3 modules of GEM before beginning the Clinical Phase of training which starts in February next year. Once again, thank you so much for the grant. It has made a great difference to my life this year and it will also help cover some of my living costs next year.
Best wishes, Jeremy Rison
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Daniel Desogus
Hi Martin, I am just contacting you for an update. I am at the end of my fourth year now and about to do my elective. I find it hard to believe that it was four years ago I was contacting you about a bursary! How have things been with you? I am thrilled to be able to tell you that I have just had my results from finals and I passed. I will start working in July/August in west midlands south deanery (I haven’t received a job allocation yet, but I am likely to be based in the Coventry and Warwickshire area). I am due to start my elective this week. I have kept it simple, and will be doing 6 weeks at George Eliot hospital with a focus on anaesthetics and ITU. I am still unsure what I would like to specialise in in the future, but anaesthetics is on my list of considerations, as well as emergency medicine, a medical specialty in hospital and general practice. I also have an interest in psychiatry but I am unsure if that is something I would want to pursue as a career. I am hoping to get a foundation placement that covers emergency medicine, psychiatry and general practice so I can experience those as a doctor and not just as a student. I would like to once again thank the Kidderminster Medical Society, and you personally, for your generous support. Without your bursary I would not have been able to afford my tuition fees in the first year of study and I wouldn’t be here today. Thank you so much, I will always be grateful for the opportunity,
Best wishes, Dan Desogus
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Kathryn Olsen I would like to start by saying thank you for awarding me the bursary. It has supported me in my first year of Graduate Entry Medicine at the University of Birmingham and is very much appreciated. I came to study medicine after working as a nurse, and had originally intended to work shifts on evenings and weekends to fund the course. However, with the support you have given me, I did not need to do this and so could concentrate fully on my studies.
Last year was incredibly intense. There was so much new information that I had to learn, including subjects that I had not covered before when I studied nursing. I really enjoyed learning all the new subjects and grew in confidence as the year went by. I also learnt how to manage my time effectively, which was essential last year. I am pleased to say that I passed all the exams for the first year and am now in year three of the undergraduate degree. I am now out in the hospital talking to patients and practicing my skills. I have been really enjoying being out in the hospital as I am able to put the theory from last year into context.
Over the summer break, I undertook some work experience with the liver research unit. This was extremely interesting, as I got to see what happens in the labs and how the research is translated into practice. The bursary I received meant that I was able to undertake this research experience over the summer, as I did not need to spend the time working instead.
Thank you very much for your support,
Kathryn Olsen
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Elective Bursary Report My elective took the form of two placements in very different locations. The first in Mseleni Hospital, Kwazulu Natal, in rural South Africa and the second at the Royal Orthopaedic hospital in Birmingham in Orthopaedics and Anaesthetics. South Africa During my time in South Africa I was exposed to injuries and diseases I had never encountered before. The first patient I saw was an infant with Severe Acute Malnutrition (SAM). The paediatric consultant was keen for me to learn about the condition as she recognised that it was unlikely I would have seen it before. This teaching took the format of a grand round. This differed from any grand round I had experienced in the UK because all the doctors attended at the patients bedside and not in a lecture theatre. The infant in question demonstrated classic symptoms of SAM i.e. she had a sunken fontanelle, reduced hair growth, abnormal breathing and was listless. Other patient interaction highlights included snake bites, which are quite common in the area. A patient I spent the most time seeing had been bitten by a Cobra. Cobras cause ecchymosis in a skip lesion distribution. I was interested to learn that anti-venom is not used as commonly as perceived. This is due to a high risk of causing anaphylaxis and it also carries a high risk of serum sickness. In additional there was a large amount of Psychiatric pathology in Mseleni. Each day on the male ward round I would see multiple patients suffering from psychosis. Patients very often would refuse to take anti-psychotic medications when they returned back to their community. Staff at the hospital also informed me that many local remedies for illnesses also precipitated psychosis. These patients were treated with anti-psychotics exactly the same as we use back in the UK. Whilst in Mseleni I assisted in hip replacement surgery for Mseleni joint disease. This is a disease that causes premature arthritis and is of unknown aetiology and affects people from the local area. All of these operations are performed under spinal anaesthetic. Interestingly a representative from the prosthesis company was present in theatre, similar to the UK, however they also brought the equipment for the operation and assisted in the procedure as a second scrub nurse.
There were many features of this
experience which were very familiar to me. This included monthly
Morbidity and Mortality meetings (M&M) which took a similar format
to those we conduct in the UK. At first the idea of attending a M&M
meeting shocked me, although on reflection I think this was my
prejudiced view of a healthcare system that I wrongly assumed would
be more primitive compared to the UK. Both here and in South Africa
we practice evidence based medicine. We strive to learn from our
mistakes and M&M meetings serve to facilitate this learning and
hopefully improve patient care. Royal Orthopaedic Hospital Birmingham The second part of my elective was at the Royal Orthopaedic Hospital (ROH) in Birmingham as I was keen to experience surgery and anaesthetics. During my time with the ROH I learnt to do spinal anaesthetics as well as honing my cannulation and airway skills - all of which will serve me well in the future. In terms of surgery I assisted in a variety of operations from knee replacements to laproscopic rotator cuff repairs. I improved my suturing skills and by the end of the placement I felt much more confident assisting in surgery. Whilst at the Orthopaedic Hospital I met specialist trainees. One of the trainees volunteered at the West Midlands CARE Team. This is charity operated in the West Midlands in which volunteer doctors, nurses and paramedics deliver enhanced care to seriously unwell or injured patients in the pre-hospital setting. I spent a day as an observer out with the charity. This was a fantastic experience that I would recommend to all students particularly those who have an interest in pre-hospital medicine. Although my elective took a different route than originally planned, I had a fantastic time in both locations and experienced a wide variety of medicine in two very different health care settings. I was lucky enough to receive a bursary from the Kidderminster Medical Society when I joined medical school and I qualified this Summer and I am now working in Derriford Hospital, Plymouth, as a Royal Navy FY1 Doctor. I must once again say a huge thank you to the society for the support I received. It makes trips and experiences like this possible and enhances students time at medical school. Dr Sam Owen-Smith
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Elective Bursary Report I would like to start with a wholehearted thanks to the trustees of the Kidderminster Medical Society for their generous bursary for my elective earlier this year. Before planning my elective, my excitement had been tinged with anxiety about how I would make the most of such an opportunity, with the limited savings I had left after seven long years at university. To have some of that burden lifted was an incredibly special gift. I spent my elective in Galle, Sri Lanka, on the South West of the island. I was placed in the Emergency Assessment Unit in Hemas Hospital, a small private hospital. Because it was a private facility, this influenced the demographic of the patients accessing the clinic, and although I did see some acute illnesses and emergencies (such as a traveller with dengue fever, several minor injuries following traffic accidents and a traveller with a facial injury from a surfing accident), I was surprised by how many subacute and minor complaints presented in Emergency Assessment Unit. It was the turn of the seasons when I was visiting so these presentations included asthma check ups, seasonal tonsillitis in young children and, perhaps most surprisingly, regular appointments for children's ear piercing! I was quite shocked by this at first until one of the nurses explained that the hospital is a very clean and controlled environment, so it actually makes a lot of sense to offer such a common practice as ear piercing in this environment, for a small fee. It was certainly a novel insight into how service provision can differ between countries or cultures, and between government and private health provision. My day to day schedule consisted of attending emergency clinic from 7 am til 12 pm, after which sometimes teaching sessions were offered; if not I began to put on teaching sessions for the other elective students, as a lot of them were pre-med or very junior students. This was a great opportunity for me to exercise some teaching skills as this isn't something I've had the opportunity to do previously. After clinic and/or teaching was over, the doctors would leave Hemas to attend ward rounds at the local government hospital, as doctors in Sri Lanka are expected to split their workload between private and government service. At this point we were allowed to enjoy our free time in beautiful Sri Lanka! I spent most evenings with friends from the hospital at the local beaches or in Galle itself, a beautiful fortress-town with much local and touristic charm to offer. At the weekends we travelled further afield, visiting some of Sri Lanka's infamous landmarks such as the ethereal hill country- oceans of tea plantations peeking out from among the mist; national parks home to herds of elephants in their hundreds; ancient cities and cultural hubs such as the colourful Kandy. Before visiting Sri Lanka I had little knowledge of the place, other than guidebooks and anecdotes from friends of friends, all of whom had attested to what a beautiful country it was and how welcoming the local people were. Often people are quick to exaggerate the positives of a destination if they know you're set to visit, but I know now that Sri Lanka needs no overselling; I had the most fantastic time. It is a truly beautiful place with more to see than I ever could have fit in, even if I wasn't juggling my travels with a Monday to Friday placement. My time at Hemas offered a precious insight into the healthcare service of a totally different place, and also gave me some insight into the differences between private and government led healthcare. I would recommend Sri Lanka as an elective or travel destination without a second's hesitation.
Izzie Dugdale
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Medical Elective Report July-August 2018, Krakow, Poland and Sydney, Australia My compulsory Medical Elective Placement was split into two, very different, halves. The first was spent watching mostly surgical procedures in the Oncological Institute of Krakow, Poland; while the second was within the Obstetrics & Gynaecology Department of North Shore Hospital in Sydney, Australia. Though both of these countries have similar resources and medical treatment compared to the UK, I came away from both having seen very different attitudes towards healthcare professionals (Poland still has an old fashioned “paternalistic” style of medicine) and different ways of running Health Services. Poland I knew that the medical practice and technologies of the economically-growing Poland would be similar to those that I was familiar with in the UK, so my main reason for choosing this country as my first stop was to improve my language skills (I am the grand-daughter of wartime Polish immigrants so my grasp is basic). Indeed, over the four week placement I became more and more confident in my conversational abilities, and even gained quite a reasonable medical vocabulary too. Perhaps my one slip up over the placement was thinking that the Polish words for “large intestine” meant “grossly obese” for a solid week. On reading the surgical list each morning I couldn’t understand why the gastric surgeons had such a plethora of obese patients! I was attached to oncological surgery, so each day was attached to theatres, and I was given free rein of each of the rooms, moving between different ones to observe the different sub-specialities. The day normally started at 6.45am, with the handover meeting (here, people talked very fast so I often had very little idea of what was going on), before getting changed for AM theatres. Even though I did not expect to have much responsibility in the way of the operations in Poland, I assumed that I would be able to do what I was used to doing as an English medical student; namely, scrubbing in and maybe assisting a little. I was to discover, disappointingly, that Poland, being a very bureaucratic country, would not even let their own residents (our equivalent FY1 and FY2) scrub into theatre, and therefore there was absolutely no possibility of my doing so! Watching the surgery itself was useful in some aspects: I was able to see lots of techniques and methods that I haven’t yet been exposed to in England. There was, for example, the removal of a fairly superficial but grotesque tumour from the chest of an elderly gentleman: the surgeons gave it a wide berth, and removed and area of skin around the size of an A5 notebook, pulling either side back together to close the hole. I have to say that the sheer elasticity of human flesh really impressed me, and once healed this particular gentleman won’t look particularly notable apart from the fact that his nipples will be very close together. I think, ironically, the most useful thing that this elective placement gave me, was a conviction that I do not want to pursue a career in surgery. After a while I did become a little bored watching similar operations day after day, and so I managed to ask for a week with the Oncological Pathology Department (housed upstairs in the same building). Here I was able to watch pathologists marking and slicing surgical biopsies, technicians making slides, and also spent time being taught by the cytology team. I felt that my Cambridge education prepared me especially well for the latter, because I was already familiar with many of the cellular markers that were being stained for. This week was probably my favourite in the whole placement, and I feel that every medical student should see at least once what goes on behind the scenes in the pathology department, and gain an appreciation of all the processes that need to be done to get that final pathology report! Australia The medicine which I witnessed in Australia was pretty much identical to that seen in the UK: there was even a huge number of British doctors, or “Poms”. My reason for going to this country was mostly for personal pleasure: I had only once ever left Europe, and wanted to explore this vast country “Down Under!” In the Obstetrics & Gynaecology department I had mostly an observant role, spending time with the consultants in clinics, residents in theatre, and midwives on labour ward. I also took histories from patients and had the opportunity to conduct a number of minor procedures myself (many pap smears and even the removal of a cervical polyp!). Two of the main highlights were unexpected: the first was a four-hour-endometriosis operation: seemingly quite boring (especially after many weeks of theatre in Poland!) but the supervising surgeon (a professor) proved to be the most enthusiastic teacher of anatomy, and he narrated non-stop during the mammoth procedure, making sure that I, and the other students, learnt at least one new fact every ten seconds. The enthusiasm and “Raw Aussie Energy” of many of the doctors I met was something to be admired. The second highlight of my placement came after spending a few days on the NICU Unit. I woke up early to attend a 7am morning meeting with a presentation about Neonatal Prematurity Outcomes. I ended up staying behind after the talk had ended, and discussed the study with the clinicians and scientists. This solidified to me how much I adore scientific research. My appetite has been whetted to be involved in the Medical Academic Community during my career. Of course, it would be remiss of me to not give space to talk about just what an amazing time I had outside of the hospital too; Sydney is one of the world’s major cities, and as a self-proclaimed “foodie” I had, culinarily, the best four weeks of my entire life. Asian Fusion food and Australian brunches made up the bulk of my diet. I also had the opportunity to visit countless museums and art galleries (The Museum of NSW was my favourite), hiked in the Blue Mountains, attended a rugby game, paddled on Bondi Beach (the water was a bit too cold in the Australian Winter), spent a weekend break in Brisbane, and went diving on The Great Barrier Reef. I met medical students from many countries: from England, Canada, Germany, Switzerland, Australia to name a few, and I feel incredibly blessed to have connected with such incredible soon-to-be-medical-professionals and now to have friends scattered all over the world.
Monika Kondratowicz
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Post Grad Bursary Report from Thoqeer Hussain First and foremost, I would like to express my sincere gratitude to Dr Lewis and the trustees for selecting me to receive this bursary. It has truly alleviated the financial burden and worries during my first year at Leicester Medical School, and for that I will be forever thankful. I was honoured to be given the opportunity to study Medicine, yet oblivious to the extent of the challenges I would be facing by studying this degree, especially as a postgraduate. I am amongst the second cohort to study the new curriculum taught at Leicester, which offers integrated teaching methods including lectures, group work and full body dissection to reinforce learning. A perk of studying Medicine at Leicester is the chance to gain very early clinical experience within a month of starting University. I was placed in a psychiatric unit for a week, followed by a week at a GP practice; where I mainly talked to patients and shadowed doctors. I particularly enjoyed the week in psychiatry, as I was able to see a range of intriguing mental health illnesses and manifestations. Academically, semester 1 involved learning the fundamental principles of medicine such as biochemistry and genetics, whereas semester 2 focused more on physiology, pathology and anatomy. A typical day consists of a morning of lectures and group work, where in groups of 8 we work through a set of questions based on what was taught in the lecture. These groups are determined by completing a questionnaire before we started medical school and formed based on our personalities- so that each person brings a different skill to the table. Fortunately, I get along well with my group and feel that we work quite well together, which has made groupwork more bearable! I previously studied Biomedical Science which was taught very differently, so adjusting to new teaching methods was, at first, challenging. I underestimated the volume of content and admittedly struggled with the fast pace of learning which was required. Unbelievably, I was screened and diagnosed with dyslexia during the first semester, and my assessor was surprised how I had gotten this far without any support! The bursary was extremely helpful in allowing me to acquire some assistive equipment before my exams, which made a huge difference. Prior to receiving the bursary, I started medical school with the intention of working part-time to fund my degree. However, the bursary enabled me to invest some of this time into joining new clubs/societies; most notably hockey and badminton. It has also helped greatly with travel expenses, as I travel back home frequently to care for an ill relative. Recently, I received by results and am delighted to have passed my first year, despite the difficulties. I aim to spend this summer taking a well-deserved break, before commencing work to save up for my second-year fees. I would like to conclude how I started, by thanking Kidderminster Medical Society for making bursaries as such available for people like myself, as without it, I would have really struggled this year. Your generosity has inspired me, and I hope you can continue supporting medical students in the future. Kindest regards, Thoqeer Hussain
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Post Grad Bursary Report from Stuart Evans
There is no other way to start my report than with a sincere thank you for awarding me the £3,000 post graduate bursary in support of my studies at Leicester Medical School. Having decided to study medicine towards the end of my previous degree, a key worry was how I would finance my studies due to the lack of student support available. The bursary has enabled me to focus almost entirely on my studies, with very little pressure on me to work part time, especially during exam time. I chose to study at Leicester Medical School as the integrated method of teaching provided many avenues to develop my knowledge; through didactic lectures, small group work and full body dissection. The first semester was most challenging for me, as biochemistry and genetics were not previously included in my paramedic training. Semester two was more enjoyable as it focused on topics such as cardiovascular physiology, musculoskeletal anatomy, immunology and pathological processes in disease. The bursary enabled me to focus much of my time on revision, allowing me to score very highly in my end of first year exams with over 90%. Leicester university also offered a unique, very early clinical experience (VECE), which saw all first year students attend clinical attachments for 2 weeks within the first month at university, following a brief training period of manual handling, infection control and basic life support. Having practiced as a paramedic for the last 7 years I felt I had a wide understanding of many areas of the NHS, however this placement allowed me to experience a week in a secure mental health hospital where I also participated in a range of patient activities. I am hoping to enjoy my summer break with my family, where I will rest and give my brain a chance to re-charge. Next year looks to be very demanding, covering details topics such as head, neck and neuroanatomy, as well numerous other systems. I have also had meetings with the medical school and East Midlands Ambulance Service, as my friend and I are hoping to set up a community first responder scheme using medical students, with an ambition to join forces with the an other local university who have a large nursing student programme. Thank you again for the very kind bursary you provided; it has certainly had a positive impact on my first year performance at university.
Best Wishes Stuart Evans
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Bursary Report from Catherine Odendaal I would like to start off by thanking the Kidderminster medical society for providing me with this bursary for my first year of graduate medicine at the University of Birmingham. This bursary has been so valuable to me in my first year and I have been able to carry forward this support as I prepare to enter the clinical years of my degree. I have been able to relax about my finances for this year rather than constantly worrying like I did before the year begun. My bursary has been able to help pay for rent and expenses and I still have some remaining which I will carry forward to support me for this year. At the university of Birmingham, the first year of the graduate entry course, the 2 undergraduate pre-clinical years are sandwiched into one. Cramming as much as possible into a single year via problem based learning. Undertaking problem based learning for the first time was such a steep learning curve. I had to learn how to navigate my role as a team member as well as a team leader. At first this felt uncomfortable, however as time went on I became more comfortable and confident in my own abilities and my contributions to each of my groups improved, supported by my mentors via positive feedback. I learnt to really appreciate the PBL process, despite its ups and downs, as I realised I was learning so much more than I would if I was in lectures. The summer exam period was particularly difficult, however I am pleased to say that I performed well in all of my written exams and also passed my first OSCEs. Despite the pressure and demands of the first year I have still been able to enjoy other activities outside my course, which is something I was determined to do before starting medicine. I have played netball for the medical school netball 4th team and have recently volunteered to captain this team for the next academic year. I also played trumpet in the medical society’s big band. On most weekends I managed to visit my husband who I unfortunately did not get to live with this last year, when visiting home I have also been able to work occasionally at a local restaurant to help save more money. This summer, I've been fortunate enough to visit Swaziland and have spent a week at a small village hospital in Big Bend. Ubombo Sugar Hospital caters for the employees of the large sugar company Illovo and their families, as well as some private patients. I've been able to spend time doing ward rounds, attending the out-patients department clinic as well as private consultations. Its been really interesting to see how such a small hospital functions on a small budget whilst providing essential care to people in the local area. Recently, with the help of my bursary i have been able to start driving lessons, which is something I have never been able to afford previously. It feels good to finally be gaining some independence. Having my license will be great for getting to my placements for the next 3 years. I have found out that my first placement will be in Hereford county hospital. I am so looking forward to entering my clinical years and starting to put my knowledge into practice and learning from patients.
Many Thanks Catherine Odendaal
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Bursary Report from George Williams First of all I would like to express my gratitude to the members of the Kidderminster Medical Society for awarding me the generous bursary. It is difficult to fully express the thanks I have for the award, £3000 is an astonishingly large amount to receive and the difference it has had on my year is monumental. I have applied for medicine several times before and have been unsuccessful hence the reason why I am pursing a career through the graduate entry course. When I received my place at Nottingham I obviously jumped at the chance, however this meant I would be moving away from my wife, who is currently studying nursing at Cardiff University. The bursary has helped significantly in the travel costs, without the bursary I may not have been able to travel to see my wife as frequently as has been possible. The majority of the money has been either used to pay for study materials or help with rent for my flat. I still have some of the bursary remaining to keep in savings to enable me to plan for any unforeseen circumstances throughout the course. The first year at medical school has been far more demanding than I had thought possible. I am used to high workloads but the difficulty is the amount of work required outside of formal teaching. I have spent many early mornings and late nights in the university working to ensure I don’t fall behind and I am prepared for exams. The amount of independent learning that is expected on a GEM course is far higher than anything I have experienced before. During the first few months I found it incredibly tempting to try to research information that was far too deep than I needed to know, however, I quickly found this was unsustainable. The teaching method of Problem Based Learning was also a very new concept to me, it essentially involves group work with a facilitator to work together to investigate an individual case. However, it forms much more learning than it may initially seem, something I quickly realised during my formative exams! During the months at the university we have covered multiple systems in what seems like a very short space of time, and it was only during the last module of the year that I was able to look back and realise just how much I had learnt. During the year, I have also been involved with the Derby branch of Nottingham Marrow, the student branch of Anthony Nolan. My role in Marrow has been to work as a volunteer clinic organiser, I have been involved in several clinics where we have recruited a large number of new donors to the bone marrow register. I believe this is a fantastic achievement particularly considering the Derby branch of Nottingham Marrow has only started this year. Finally, I have also started the Nottingham Advantage Award, this is a course that enables me to enhance other aspects of my life, with the aim of becoming a more rounded individual and doctor upon graduation. I aim to start learning basic British Sign Language next year, which will undoubtedly come in useful in the world of medicine. Some of the courses do require a small fee to take part and therefore I plan to use some of the bursary for this purpose. There are so many ways the bursary has and will continue to improve my time at Nottingham and I believe I would have found my time here much more difficult without it.
My sincerest thanks, George Williams
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Bursary Report from Ben Ryland
I would like to start by thanking the members of Kidderminster Postgraduate Medical Society for awarding me this scholarship; my gratitude is difficult to put into words. The award was used to help different aspects of my first year at Aberdeen University; the most important to me by far was having enough money to travel home to visit family members when needed. Studying this year has been demanding and having the chance to see my family without worrying about the cost of travelling was amazing. The majority of the award was used to help pay the rest of my tuition fees and rent when needed. The latter came in handy because I still kept my part time job whilst studying to pay rent each month, but took time off work when exam season came about, so it was nice having money to compensate for the lack of hours at work. The first year of Medicine at Aberdeen University has been difficult but rewarding, the most challenging aspect was the difference in learning styles from my first degree. Because of the content load I found myself constantly having to stop delving deeper into the material to gain further understanding, which was necessary in my first degree. The first term focused on raising every pupils understanding of biological principles to the same level; major topics covered included Biochemistry, Immunology and Anatomy. These topics weren’t particularly challenging because a lot of the material was covered in my first degree. Second term however introduced systems based learning, covering the respiratory and cardiovascular system. I thoroughly enjoyed this term because we covered pathophysiologies as well as anatomy and normal physiology, attempting to disease presentations as well as treatments and management. I mentioned above that I spent a lot of first year working, which came with its own challenges. I found my part time job within the first week of moving to Aberdeen and managed to work about 20 hours a week. This meant that I didn’t have much time for social activities, and I was left feeling a little excluded from people on my course, this led to some struggles. The scholarship really helped by allowing me to work fewer hours, so I could take some time to make friends and begin to enjoy my time at Aberdeen. Again, I am so thankful for having received the scholarship as It made my first year experience so much better than it could have been.
Thank you. Ben Ryland
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Bursary Report from Karnjit Johal
Firstly I would like to thank everyone at the Kidderminster Medical Society for the bursary I received whilst studying in my first year of the graduate entry medicine course at the University of Birmingham. In the first year of study, students are expected to pay £3,000 towards their studies as tuition fee loans do not cover the full amount, so I had intended to work evenings and weekends during my studies to be able to fund this. Receiving the Kidderminster Bursary meant that I did not have to worry about this and not only gave me more time to study but also reduced the stress of working so many hours alongside my studies. The course as you can imagine was quite intense and challenging as it involved teaching 2 years of undergraduate studies in to one quite compact year. I was pleasantly surprised in the first few weeks as we were attached to a General Practice straight away enabling us to interact with the wider community and also allowed us to relate the theory of a condition to a real life example. This helped considerably when it came to exams as I would remember not only the condition but the patient that presented with it and their story. GP placements were also a place where we developed our clinical skills such as taking blood pressure and systems examinations which we could then carry out with patients to further enhance our learning. The rest of the week was spent working in groups in a Problem Based Learning (PBL) format and self-directed learning. This was the first time I had experienced PBL, but it worked very effectively as we could bring our knowledge from the variety of previous degrees and discuss any gaps in our knowledge and then research them and present back. This structure allowed me to learn and understand the curriculum as I worked through the PBLs which made revision less stressful towards the end. The first two modules studied were ‘Cells and Cancer’ which involved learning the cell cycle, the most common cancers and their pathophysiology and we then covered the cardiovascular and respiratory systems in ‘Supply and Demand’. These were examined in the first two months and thankfully successfully passed. We then moved on to Neuroscience and Immunology which proved to be both fascinating and challenging. It was at this point that group study sessions on weekends became key to understanding topics as we could all pool our knowledge and research together to try and take on the anatomy of the brain and immune system and the pathophysiology of the conditions involved. We quickly realised that learning and teaching within a group significantly helped understand the topics better. Once the second set of exams were completed and passed, I became confident in the PBL process and had gotten used to the routine. After the new year, we began ‘Loss and Renewal’ and ‘Fuels’ which covered the reproductive and gastrointestinal systems respectively. At this point OSCEs were fast approaching and any free time was spent examining one another in order to prefect our skills. Having worked within a retail and admin setting for the past 6 years I was able to further enhance my existing communication skills, and using the clinical skills rooms at the university made the whole experience more realistic. I am now a third year clinical student and still cannot believe how much I learnt and was able to achieve within the last year. I am grateful to the Kidderminster Medical Society as without the financial support, last year would have been far more challenging and stressful.
Once again, many thanks Karnjit Johal
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Dear Dr Martin Lewis and the trustees of the Kidderminster Medical Society, Re: Tom Brookes bursary award - report of academic achievement for year 2015/2016. I am writing to say a big thank you for the financial support towards my Medicine degree at University of Manchester for the academic year of 2015/2016. It was a fantastic help and was greatly appreciated. I passed my first year having achieved both Satisfactory and Honours in the two academic exams and a Satisfactory in my first ever OSCE (Please see table below for a more comprehensive break down of results) I have thoroughly enjoyed my first year of studying medicine. My first semester was titled “Life Cycle” and covered everything from fertility and embryology to cancer and osteoporosis. A very varied semester with many interesting aspects. My second semester was titled “Cardiorespiratory Fitness” and covered the cardiovascular and respiratory systems in great detail. I also experienced my first ever OSCE examination. I am aware that some universities don’t give their students OSCE’s until their clinical years, so I am grateful to Manchester University Medical School to have given us the opportunity to prepare for later years by giving us OSCEs this early on in the course. Studying for a degree in medicine has been a completely different experience to studying for my previous degree. It is an incredibly fast paced, challenging but also thrilling rollercoaster of a course. I have experienced academic learning at a pace never experienced before, as well as developing communication skills by talking to simulated patients and real patients in GP and Hospital placements. I absolutely love this course and again count myself so lucky to have been given the opportunity to study medicine. Again, I’d like to express sincere gratitude to you and your fellow trustees for the grant you awarded me. It has helped me tremendously and took a great weight off my shoulders.
Yours sincerely Tom Brookes
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Bursary Report by Daniel Desogus (Summer 2016) Dear Kidderminster Medical Society, Firstly, I would like to thank Dr Lewis and the trustees of the Kidderminster Medical Society for choosing me to receive the bursary. It has helped me immeasurably and I am so grateful for it. I started my first year at Warwick Medical School in September last year and I really can’t believe how quickly it has flown by. It has not been an easy year. I have sadly lost several family members in the last year which added to an already difficult year. Along with the accelerated structure of a graduate entry medical course, it is the hardest I have ever had to work, but I have thoroughly enjoyed my first year at Warwick. I sometimes still cannot believe I am at medical school or that I have just finished my first year. Being a doctor has been something I have wanted for as long as I can remember and I finally feel like it is within reach. Warwick only offers a graduate entry programme for medicine, so the intake for the course is larger than some other universities who only have a limited space on their graduate entry programme. A big advantage to this is the huge diversity in student backgrounds that there is there. Students were of all ages, with different levels of experience and previous degrees in a large variety of subjects. This meant that colleagues on the course all had their own unique perspectives and ways of thinking, which helped a great deal in the case based learning sessions. The case based learning system at Warwick falls somewhere in between a traditional taught course, and a problem based learning course. The year is split into five subject area blocks which last five weeks each. Students are split into case groups at the start of the year comprising of eight or nine people and a member of academic staff who acts as facilitator. Each week a new case is given, with three group sessions for each case and new information released each session. Within the group we set our own learning objectives each session and split them between group members, who would then have to present their topic at the next session. These cases were supplemented by lectures which (usually) were related to the body system covered in the case. At first I was sceptical over case based learning. Experiences with case studies in my previous degree hadn’t been overly successful. Although enjoyable, I found it difficult having to rely on other group members, who sometimes were unreliable or didn’t put the effort in. However, this year my opinion has been completely changed. I thoroughly enjoyed group sessions and as a group we grew, improved and bonded. Everybody was reliable and put the effort in, which resulted in me learning a great deal from these sessions. Everybody also had something to bring to the sessions, with different backgrounds and areas of expertise, meaning we all managed to benefit from working together. Learning was split into five blocks. Block one covered homeostasis and metabolism. Block two was blood, lungs and heart. Block three was brain and behaviour. Block four was locomotion, muscles, bones and skin. Block five was reproduction and child health. Throughout these blocks core themes were taught covering anatomy and imaging, physiology, pharmacology and cell and tissue biomedicine, as well as values, law, ethics and social and population medicine. Along with this we spent Friday’s at University Hospital Coventry & Warwickshire where we had anatomy, radiology and clinical skills teaching. The anatomy at the hospital was based in the surgical training centre where we mostly used plastinated specimens that related to the body system we were currently studied. Although the plastinates were excellent for pointing out structures, they didn’t compare to the occasions when we had real tissue to study, which were always fascinating and one of my favourite things to study. Clinical skills training was taught in small groups and involved discussion and teaching of an examination or skill, followed by practice within the group. We covered many skills, learning at least one new one each week. Clinical skills covered included less invasive examinations such as systems exams and blood pressure, as well as history taking both within the group and with simulated patients. We covered many skills throughout the year, however it didn’t really sink in just how many we had learned until it came to revising for OSCE’s and realising just how many things there were to cover. Clinical experience with patients initially started within the first few weeks when our case groups each got assigned to a community placement. Our group was based in Atherstone, a very small town in north Warwickshire. Our tutors there were two excellent district nurses who both lived locally and knew the area and patients well. We had several days based there, where we initially started by learning the area and researching the town and population, before moving on to seeing patients. We saw three patients there, with each half of the group seeing a different patient. Patients were chosen so that we each saw an infant, an adult and an elderly patient, each with a chronic illness. We had time speaking to patients in their own home and also spoke to family members and staff from various agencies responsible for their care, including district nurses, GP’s and carers. The emphasis was not on the patient’s symptoms or treatments, but on how the illness affected the patient’s lives. We then had to prepare a presentation for the other half of the group explaining what we had learnt from each experience, how the patient’s life had been affected and other possible agencies that we think could benefit them. Each patient we saw was an eye opening experience and I found the days to be enjoyable and hugely beneficial. It added a personal perspective that can often be lost in a clinical setting or in lectures and emphasised how an illness can affect somebody’s life, as well as the lives of their family. After Christmas we had clinical placements for half a day each week at one of the local hospitals. I was based at George Eliot hospital. It is a smaller hospital than UHCW, however groups were smaller meaning everybody got to do more and spent more time with supervising doctors. Groups were taken around the hospital by a supervising clinician, where we were taken to patients and had the chance to take histories and practice clinical skills. Clinicians would also teach us better techniques or ask questions, as well as helping to link knowledge from lectures to the clinical settings. Each week I saw a different clinician with a different specialty, meaning I got to experience different areas of medicine, practice different skills and learn about different systems. Some of the clinicians had also prepared presentations or learning materials as well which were always informative and helpful. Whilst on clinical days, we had to prepare two written presentations which covered diagnosis, treatment and a short essay that involved research into evidence based medicine. I really enjoyed the clinical days at the hospital. It gave a true taste of what it is like to work in a clinical setting and helped develop skills further, as well as helping me to tie skills from different areas of learning together. Revising for exams was difficult. We had formative exams at the end of each block, but these didn’t count for anything and were just so we could judge how we were progressing. There were no Christmas exams, so the whole year came down to a two-week period in the summer. There was such a large volume to get through and it felt like I could never learn it all. The exams themselves were long and covered such a wide area and even after written exams were finished I couldn’t relax because OSCE’s were the following week. However, I found OSCE’s less stressful as we had so many opportunities to practice them. Even though I walked out of exams feeling like I hadn’t done badly, I still didn’t really believe I had passed until results day. When results came out I was thrilled to have not only passed, but to have passed well. I finished the year by going on holiday with my girlfriend. She has just finished her final year at Hope University in Liverpool, so we have both had challenging years. We enjoyed the chance to relax and spend time together, as we hadn’t seen each other as much this year due to the distance and workload. The last year has only strengthened my desire to become a doctor and I am now due to start second year in September. Second year should have even more time in a clinical setting, as well as learning more procedures and more complicated cases. My girlfriend is moving down to Coventry to get a job and to live with me and we are getting a house together and I am really looking forward to the year ahead. Finally, I would like to thank you all again. I do not think I could have found the money required to pay my course fees in time if it had not been for your generosity. It has helped me pursue the only career I have ever wanted and I will always be thankful for that, Yours sincerely, Daniel Desogus
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Bursary Report From Lucy Studd October 2015
I would like to thank everyone at the Kidderminster Medical Society for the generous bursary I received at the start of my studies on the Graduate Entry Programme at St George’s, University of London. I had a fantastic, very challenging year, and sometimes still can’t believe I’m here and training to be a doctor. It’s a pleasure to let you know how I’ve been getting on. At St George’s, like other graduate courses, we race through years one and two and, afterwards, join those going into third year. What I think is great about training here is they get patients to come in and send you on GP attachments from week 1. We were able to apply our growing knowledge to real people. I loved meeting patients and putting what we were learning into practice. We started with Life Cycle, looking at everything from reproduction to palliative care. I found the module really interesting, and started to see how I learned. Throughout the year we had weekly anatomy sessions in the Dissecting Room. They seem to be a bit love-them-or-hate-them, but I find them really useful. Peer tutors and core trainee surgeons teach us, and there’s little better than passionate people passing on their knowledge. It also means that from third year onwards, we can apply to gain teaching experience ourselves. As a graduate I really appreciated the PBL structure and focus on self-directed study; reporting back what you’d learned twice a week to a small group. Revising for the first set of exams before Christmas started during the second module, Life Protection. This was immunology, genetics, and cancer…the sensation of doing a marathon at sprint pace set in, and I felt keenly aware of being an arts graduate and had moments of ‘imposter syndrome’. These exams were going to show that I had no right to be here. Admissions had surely made a mistake. Luckily, I have been made some fantastic friends on the course, and through group study sessions, often late into the night, began to see that everyone felt that way, for whatever reason. Everyone finds different parts of the course hard. I’d heard people say that medicine is a team sport, and it really started to become apparent. You just have to work through it, but often it’s best to do it with others. With the first set of exams over and done with, the new year got under way. I gained a place on St George’s University Challenge team! I can’t say too much as this series is still running… but we made it through to the television rounds and filmed in Manchester at the beginning of 2015. It was such a fun experience. St George’s is a small university, and it focuses on healthcare, so we were really pleased to have the chance to represent the other students and demonstrate a few other fields of interest! We rushed back from filming to our second lot of exams, and after a short Easter break, headed into the final term; the final exams and our OSCE. My grandfather, to whom I was very close, became very ill and passed away. I went home when I could and when back in London I found it hard to concentrate. My personal tutor gave me advice and my friends helped me catch up things I’d missed, though it was only really after the funeral that was I really able to see how supported I had actually felt. It helped to keep busy, and I distracted myself with work. Also around this time I and three other students co-founded the St George’s Athena SWAN Students Network; a Women’s Careers network. Our aim is to encourage women to believe in and push themselves, to excel, and to introduce them to role models so they can set their sights high. We have our first event this November. I’m really excited to see where we can take the society and how we can help other students at St George’s. By the end of the academic year, we knew we were running on fumes, but the routines and camaraderie that we had developed really helped. Before medical school, I was an actress. Everyone said I would be confident when the OSCEs came round. I couldn’t believe how much more worried I was than before any audition I’d ever had! I could see how much it all meant to me and how much I wanted to do well. I finished the year in the top decile and with a Merit in Medical Sciences. At the beginning of the year I would have been happy to just pass, so I was absolutely delighted. It really felt like all the hard work had paid off. After a challenging year it was great to relax, go on holiday, and finally see the family and friends who’ve been so supportive for the last year. I’ve now started back at school as a third year! I really looked forward to studying again, and after a brief introductory module, started a 5-week placement at a GP practice. It’s been great to see just how much we’ve learned in a year. I felt like I was kept on my toes; any patient could walk through the door, I could need any one of the clinical skills we learned last year. Working daily with real patients has made me really look forward to my upcoming medical and surgery placements. Studying in London brings with it the added issues of much higher rents and living costs. The peace of mind that has come with knowing I would be able to afford the first year’s tuition fees and be able to put extra money towards my rent every month for a while has certainly made things easier. I can’t thank the Kidderminster Medical Society enough for the bursary. I was speechless when I was awarded it I really appreciate how much I’ve been able to since then. Kind regards, Lucy
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Dear Kidderminster Medical Society
I would like to express my sincere thanks for the generous grant you gave to support me in my first year of study at Birmingham University. It really was such a privilege to have that extra financial security during my GEC year, and it meant that I could wholeheartedly embrace everything that being a medical student has to offer, as I will try to illustrate below. |
||||||||||||||||||||||||||||||||||||||||||||||
|
The first year of the Graduate Entry Course (GEC) at Birmingham University attempts to get us up to speed with the first 2 years of the undergraduate course, so I was well aware that it was going to be an intense year. We undertook modules in Cells and Cancer, Cardiovascular and Respiratory systems, Immunology, Neuroscience, Reproduction, and Gastroenterology and Metabolism, along with anatomy teaching and aspects of medicine in society such as Psychology, Sociology and Statistics. We also spent one day a week in a GP surgery, which was definitely my favourite day of the week. It was rewarding to see the elements that we were studying applied to real patients, and to gain a greater insight into patients’ experiences.
|
The Group at 5600 mts
|
|||||||||||||||||||||||||||||||||||||||||||||
|
Obtaining patient's vital signs
|
While the workload was massiv, I thoroughly enjoyed all of it. My previous degree was Natural Sciences, with a masters in cancer genetics and statistics, so most of the learning material was brand new to me and I was constantly stimulated. It’s incredible to look back and see how steep the learning curve is! It’s also petty impressive to see the vast folders of notes that I made in just a few months. The examination period was long and exhausting but it was a great relief to get pleasing results and know that I could commence clinical placements this September. I am looking forward to the hospital side of medicine this year as well as more community based medicine in a GP placement setting.
|
|||||||||||||||||||||||||||||||||||||||||||||
|
Last year was not only work related though. I moved back to Birmingham, where I grew up, and I was grateful to have the opportunity to rediscover my home city as an adult. There’s lots going on in Birmingham! I was also invited back to my school to give talks about studying medicine as a graduate, which most people don’t realise is a positive choice. As a keen sportswoman, I continued my triathlon training and participated in the Birmingham half marathon and the City of Birmingham triathlon last year, which I have no doubt I will do again this year too. I also joined the Wilderness Medicine weekend away in Snowdon to learn some expedition medicine skills and climb mount Snowdon. It was a great opportunity to meet medics from other years and combine my interests in medicine with my love of mountains. |
The very busy pharmacy
|
|||||||||||||||||||||||||||||||||||||||||||||
|
The annual village school trip to the doctor
|
Before starting medicine I worked with a youth charity in East London for a year with underprivileged young people affected by gangs. I am passionate about empowering young people to make positive lifestyle choices, so I have taken the opportunity to join in with several societies that the medical school has which team up with local schools. I have taught mental health lessons in secondary schools with Birmingham Med Minds, and I have attended talks run by the psychiatry committee about Child and Adolescent Mental Health. I also attended an evening conference in London run by the youth charity XLP in partnership with the mental health charity Young Minds about Tackling Youth Mental Health. This year I will attend a CAMHS conference in September, and I will continue to take opportunities to teach with Birmingham Med Minds. I am also co-ordinator for the volunteering organisation Sexpression, which trains student volunteers to teach Sexual Health education in local secondary schools. It is a privilege to be leading an enthusiastic committee and I am looking forward to all that this year will bring, including the national Sexpression UK conference in November. I also hope to join the society Street Doctors, which teaches first aid to youth in gangs in Birmingham. I’m grateful to be able to tie together my experience in youth work with all the opportunities that beinga medical student presents. |
|||||||||||||||||||||||||||||||||||||||||||||
|
One of the most significant things that I used the grant money for was a medical expedition this summer to the Himalayan Ladakh region of India. I have trekked in this region twice with my family, and I was always shocked by its remoteness – the whole region is above the Himalayan tree line (3000m above sea level), and local inhabitants have to trek 3 weeks to get to the nearest doctor. Even then they are cut off for 7 months of the year due to heavy snowfall. When I was accepted into Birmingham medical school I began researching ways that I could be involved in delivering healthcare to this area and I was delighted to come across Himalayan Health Exchange – an American/Indian based company which enables doctors and medical students to undertake a medical expedition here every year. This August I joined a group of 29 doctors and medical students from around the world on a challenging trek and an incredibly rewarding experience. Over the course of three and a half weeks we saw over 600 patients, trekked over 120 miles, ascended up to 5600m above sea level, and made lifelong friends. We learned from each other during evening presentations, we were able to take on our own patients and come up with a management plan, distribute medications from our mobile pharmacy, and also experienced first-hand the medical challenged of being at high altitude. I have attached some pictures below which I hope speak louder than words. |
Not your average consultation
|
|||||||||||||||||||||||||||||||||||||||||||||
|
!
|
Before I began the course I was warned that it would probably be the most intense and miserable year of my life. While the workload was heavy, I would certainly argue that the last twelve months have been some of the very best – I’ve begun a course that I know I will continue to enjoy and will open so many doors to use the skills and experience that I am gaining, I’ve settled in to this city and most importantly I’ve made some treasured and lifelong friends. |
|||||||||||||||||||||||||||||||||||||||||||||
|
Once again, thank you very much for such a generous grant. Claire Wallace
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Dear Dr Lewis and trustees of the Kidderminster Medical Society,
I would like to thank you for the bursary I was awarded by the Kidderminster Medical Society at the beginning of my first year of medicine at the University of Southampton.
I have just successfully completed my first year of graduate entry medicine. Prior to starting the course I had an idea of the challenge the course posed having spoken to friends and colleagues during my previous work as a theatre assistant at the Royal Orthopaedic Hospital in Birmingham. My perception of the course however was not a true reflection of how demanding the course would be, and also did not reflect how rewarding I would find the course.
During my first year we focused on four major systems: respiratory, cardiac, renal and gastro intestinal. This was combined with clinical work placements at Winchester hospital. These sessions for me were definitely the most interesting. It allowed me to apply the knowledge learnt in lectures whilst studying the topic week. As you can imagine covering such a wide range of topics was very enjoyable but at times also a stressful process. I imagine this comes with the territory.
I was very privileged to receive the bursary which meant that financially I did not have to worry quite so much, especially given that a proportion of my tuition fees had to be self-funded. This meant that I had to find a much smaller amount of money and really meant I could relax before undertaking this difficult year.
Once again I would like to say a huge thank you for the help this bursary afforded me. A letter seems a meagre response given the amount of money awarded to me. If there is anything else I can do please do not hesitate to ask.
Yours Sincerely, Samuel Owen-Smith
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
To Kidderminster Medical Society,
First of all I would like to thank you for the grant that your society has given me, it has truly helped towards paying my tuition fees this year. This year has been fantastic. Deciding to carry on studying to do medicine after my nursing degree is one of the best decisions that I have made. I have found that I am really interested in what I am learning and keen to learn more. During first semester this year we have covered the life cycle. This included everything from learning about the foetus and conception to learning about frailty in the elderly. As medicine at Manchester is taught using a PBL style this means that each week I get a case and then go away and learn about the disease or normal physiology presented in the case. This is complemented by lectures and anatomy sessions. The PBL style has been extremely helpful as it has meant that I have learnt the content well and understood it fully. In my semester one exam I received honours and in the progress test I received distinction. For my second semester the focus was on the cardiovascular and respiratory systems. I particularly enjoyed learning about COPD and asthma in more detail as these are conditions that I came across everyday in nursing but didn't understand them in detail. During this semester I also wrote a literature review on emergency contraception and its effectiveness particularly in overweight patients, which again I found stimulating. At the end of the semester I achieved satisfactory in my semester test and honours in both my progress test and practical OSCEs. Throughout the year I have been involved in a society called HEAL for which I am secretary. This society aims to bring together the different healthcare students at Manchester to encourage better team working when we all get into practice. This year we have organised three events. The first was in first semester and it was a lecture on palliative care. For the event we had speakers from each healthcare speciality talk about their role in palliative care. We had over 250 students at the event and the evening was a big success. For our second event we had a pub quiz where healthcare students could come and interact with each other in a more informal situation. Finally, we hosted a clinical skills event. This involved different stations where students could learn, amongst other things, emergency resuscitation, how to deliver a baby in an emergency and what to do in the event of a prescribing error. Each station had a nursing, speech and language therapy, medicine, midwifery and pharmacy student and by the end of the evening everyone was interacting which made it worthwhile. In addition to working with HEAL I have been on the board for Manchester University’s Education Across Professions (EAP) group. This is a group of staff that are trying to get education across professions into the curriculum in the various healthcare courses. As the student representative I offer my views on potential projects and help to suggest what would be helpful from a students perspective. I feel that by being in this group I can hopefully help to make a difference at Manchester and help to instil team working in Manchester healthcare students. Finally, but by no means least I have been on the universities jazz dance team in which I travelled to other universities and competed on the weekends. This was loads of fun and a great way to relax! Next year I hope to continue my involvement in HEAL and have been elected as joint chair for the next academic year. I will also continue to contribute to the EAP meetings and hope to be in a dance team again. During the summer I have a job as a nurse so I can keep up my skills and training and also earn a bit of money on the side! Thank you so much once again for your generous support this year, it really has made a difference.
Yours Sincerely, Laura Cowell
|
||||||||||||||||||||||||||||||||||||||||||||||
|
This time last year I received a substantial bursary from you. I believe this award had a significant impact on my enjoyment of the previous year and my subsequent achievements. I hope this report goes some way in demonstrating how grateful I am. Being financially secure affords both time and opportunity that would otherwise be spent working to make ends meet. You may well be aware that tuition fees are now £9000 per year and tuition fee loans only cover £6000 in the first year. Students must therefore find £3000 from their own pockets during their first year at medical school. I personally would otherwise have had to of taken a part time job to find this amount of money. Upon starting graduate entry medicine I had (perhaps foolishly!) chosen to finish the lab work towards my PhD early and write up during my first year of med school. The shortened 4 year course at the University of Southampton is based on the problem-based learning (PBL) system which presented a new style of learning and a significant challenge due to the breadth of subject and accelerated nature of the course. I was fortunate in having some great friends on the course, who helped me in covering and understanding the course material, and the time your bursary afforded so that I was able to pass all aspects of my first year at medical school. I completed my PhD thesis, passed my viva with minor corrections and, in the last year, I have first-authored publications in the New England Journal of Medicine and the American Journal of Pathology and co-authored publications in PLOS Medicine and Endocrinology. This would not have been possible if I had also been working in a part time job. The bursary you granted me also allowed me to take two, one-week, electives at the Liver Transplant Unit at St. Vincent's Hospital, Dublin, Ireland in December and August. Having spent 4 years during my PhD attached to the liver transplant unit at the QE Hospital Birmingham from a mainly academic perspective, these were amazing opportunities to see the clinical side of hepatology and to get a real sense of what the job of hospital doctors entails. I wouldn't have been able to achieve all of these things or take the opportunity to pursue electives without the time and freedom the Kidderminster Medical Society bursary afforded me and I am incredibly grateful and indebted to the society and its donors for this. The bursary made a huge difference to my first year at medical school, as I'm sure it does for all recipients, and long may it continue to do so.
Yours sincerely, Laurence Hopkins
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Firstly, I must begin by saying what a privilege it is to have been given a place studying medicine. My first year of medical school has gone by so quickly and it seems crazy that I am already one month into my second year. The year constantly threw surprises at me, especially when I went onto the ward for the first time to take a patient history from a lady who had been diagnosed with breast cancer. Soon after my initial questions I realised that I had been sent to the wrong patient and this patient did not have breast cancer but had actually been admitted to the emergency department following a suicide attempt. This taught me very early on that you never know what each day is going to bring in the medical profession and you have to be ready to think on your feet. Although, this is definitely challenging, it is also an aspect that I thoroughly enjoy. Having studied biomedical sciences previously at Cardiff University, it is really rewarding to be able to apply the knowledge I learnt and am still learning to a clinical setting. I have most certainly found studying medicine a lot more challenging than my undergraduate degree, as being on a graduate-course there is a lot more self-directed learning expected. My first year included studying both the respiratory and cardiovascular system; whilst studying different aspects of these systems in my previous degree I started medicine thinking that I would most likely want to specialise in cardiology and not the biggest fan of the idea of respiratory. However, having now experienced these specialties clinically on the wards, I have completely changed my mind and am a strong lover of the respiratory system and related pathologies and not so keen on cardiology. The summer examinations were hard, mainly because I wasn’t quite sure what to expect in the exam, I found it was very clinically orientated, enforcing you to apply what you had learnt throughout the year to clinical scenarios. Fortunately, I passed and was very happy with my results, finishing the first year on a very good note! I cannot express how grateful I am for the bursary from the Kidderminster Medical Society as this has helped me dramatically; especially at Christmas time when my laptop decided to give up and I was left computer-less with a coursework deadline looming over me! In addition to the academic side of my first year studying medicine, I must also emphasise that I have met some truly wonderful people on this course and hope to call them friends for life.
Shannon Lennock
|
||||||||||||||||||||||||||||||||||||||||||||||
|
My name is Alice and I was the recipient of the Kidderminster post-graduate bursary at the beginning of the last academic year for Graduate Entry Medicine at Birmingham University. I am writing primarily to send my gratitude and to also give a small report on how the year has gone. Having the rare luxury of financial security to cover living expenses for a whole academic year, in probably one of the most challenging years of my life so far, was extremely helpful and enabled me to really concentrate on my studies. So thank you very much! GEC medicine is certainly not for the faint hearted, and although I’d heard from various sources that it was going to be a tough year, I don’t think I could have ever really imagined what it was going to be like. In approximately 30 weeks we covered what seemed like pretty much all the bases of medicine on a whistle-stop tour: cancer and cell biology; the respiratory and cardiovascular system; the gastrointestinal tract and the immune system; the nervous system; endocrinology and then reproduction and pregnancy. Every week through the Problem-Based-Learning (PBL) framework, we tackled various problems in groups of 8, discussing physiology and biology; as well as trying to elaborate on psychological and sociological issues. I do agree that PBL is a good way of learning as it prevents students from mindless note taking in lectures, which does not encourage independent learning. For 3 days of the week we had to talk about what we had researched without notes, which meant that we needed to have understood and memorised information in order to be able to contribute to discussion. If any difficulties arose over the course of a group session, these could be unpicked and clarified with fellow peers. Because GECs (as we are called) are from various fields of science and expertise, we could help each other out. It is certainly an advantage to study alongside others who have different and interesting previous life experiences and educations, as is the case with GEC medicine, and I was sad to read in the student BMA recently that some medical schools are thinking of stopping their Graduate medicine courses. I can see my friends that I have formed on the course becoming excellent doctors in the future. Before commencing GEC medicine at Birmingham, I studied Biology at the University of York, and then I worked as a Health care assistant (HCA) on the Clinical Decisions Unit at the Queen Elizabeth hospital in Selly Oak. It was an incredibly insightful job that I would encourage anyone to do who is considering a career in health. I valued being able to talk to the patients and spend time giving them personal care to help to make them feel comfortable on the ward. I have signed onto the in-house bank of HCA staff, and in the Christmas holidays I was able to work a few shifts on the ward. I think the manual handling and communication skills I learnt through being a HCA will be really useful to me in the future. Now I have started my 3rd year, I am seeing a lot more of the clinical side of Medicine, and I find being in Worcester hospital on placement very exciting. I am based on the Gastro-intestinal Unit for my first medical rotation, and then I will move to vascular surgery after about 6 weeks. I am not sure what kind of doctor I want to be once I am eventually able to specialise, but I know there is lots of time to think about this over the forthcoming years, and I am excited to think of the many options which might be available to me. A dream of mine is to work with an international humanitarian aid organisation such as MSF or the British Red Cross. Alternatively, if I decide to stay local, I would like to work with refugees in the west midlands as I am aware of their plight in accessing health care services. Currently I am looking into learning Hindi or Urdu from scratch, as I have a passion for Indian culture having travelled to India a few times. I think it would be useful to have a basic grasp of a widely spoken language in a city such as Birmingham, with a wonderfully vibrant ethnic mix of people. As you might imagine, I am already looking forward to the chance to go and work abroad in my 4th year: every week I change my mind about which country I would like to spend my elective! So all in all, I have had a very challenging, yet exciting start to my medical career, and I have met some very inspiring people in the field. I would like to finish by again saying thank you to the Kidderminster Medical Society for the bursary I was given in my first year of my studies. Yours truly Alice Jones
click to go to Index at top of pag
|
||||||||||||||||||||||||||||||||||||||||||||||
|
I can’t believe how quickly this year has gone. Only a week ago I found out that I have passed all my exams and will progress into year 2, though it still seems as if I have just started medical school. I look back at this year, and it is now that I realise how much I have learnt and developed since last September, whereas leading up to my exams only a month ago, I felt the complete opposite. Last summer I was so excited to start University to start learning to become a doctor, and although some of that excitement is still there, I’m now more excited about other things, like upcoming placements and meeting the new intake that will be starting in September. Swansea University is still a relatively new medical school and this year for the first time had four years at the school (before in 3rd and 4th year you went to Cardiff) and had its first fully-fledged graduates (as before people graduated from Cardiff), which was very exciting. There was a special ball in October to celebrate this, which was wonderful and very well organised by the Medsoc, and a great opportunity to meet the years above. As a new, as well as quite small school, the clinicians and teachers are very enthusiastic and most of them know you by your first name by the end of the first term, which was very comforting leading up to the first lot of exams. It was also useful when it came to our first placement in March that we knew some of the people we were working around. My placement was in Burns and Plastics in Morriston hospital (a tertiary centre), and was a fantastic opportunity to not only see what went on, but to also practise some of our history taking and clinical skills we had learnt over the year. Though I’m still at the beginning of my career in medicine, these placements are very useful for not just learning, but also helping us to decide what specialty we would like to go into later, and my placement has perhaps pointed me away from the direction of surgery at this moment, though this could all change in years to come. I’m very happy at Swansea, as it’s not just a great place to study medicine; it’s a beautiful place to be when you want to do something not related to medicine. With beaches almost right on your doorstep and the Gower just a 15-minute drive down the road, we tended to take full advantage of the nice weather, and especially the lovely summer we had, and would head down to the beach for a day or afternoon after lectures. Looking to next year I’m quite nervous about how much extra work and responsibility we will have. On the other hand, we will have more opportunities out in clinical placements, which I am excited about and look forward to finding out where I will be placed in my next placement just before Christmas. Finally, I would like to say a great big thank you to Kidderminster Medical Society for their support through this year and I hope they can continue to support medical students in the future. Medical school was a big thing to adjust to and there are many worries going through your mind, including educational, social and financial. Though for KMS to help put your mind mostly at ease financially, I found that I could put more of my efforts into getting a good educational result and having a strong social support network at the end of my first year. Stephanie Bareford
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Carly is a local girl who is a medical student at Leicester University. The past year has been a period of my life that I will never forget. To be given the opportunity to be a doctor is something I still find very humbling, and to know that people will eventually be putting their trust in me to improve their health gives me a feeling that I can't describe. The whole world surrounding university and my placements has been fantastic. I can honestly say I have loved every minute of it so far; granted there have been days when my patience has been tested, I have missed "home" at times, and I have thought that 24 hours is never enough to get everything done that I have needed to study or read up about. But on the flip side of that, being in the hospital environment and meeting the patients gives you a sense of achievement, when they tell you about their condition, and you understand what they are talking about, rather than asking them to explain what they mean! And by observing their "characteristic" signs and symptoms, you remember that patient with how they walked, or the distension in their abdomen, far more than reading a list in Kumar and Clarke! All the patients have been lovely, all eager to help you in your progression of learning, and enjoying the company that you offer them! At university the lectures have been informative, and the addition of having guest lecturers in shows you how far you can progress with your knowledge once you have qualified. But the part that has been invaluable for me has been the addition of having a dissection room. Learning anatomy can be repetitive, and difficult to visualise from a book, but having a cadaver to look at, and see how everything connects, and fits together has been great. "Charlie" (as we felt giving our cadaver a name gave him more respect) has become the extra member to our group learning, and he has given each of us the same amount of help with our studying as any of the other group members! I am looking forward to going back to university in September, and eager to learn more. The past year has been enjoyable, interesting yet hard work, but it was made a lot easier by the bursary which the Kidderminster Medical Society kindly gave me, financially it has helped tremendously. I am a mature student, on the wrong side of 30 now, and I feel I have taken the biggest step in giving up full time work, leaving my partner to support the house and mortgage on his own so I can go to medical school. But its a choice I wouldn't hesitate to do again. You only get one shot at life, and the more I have seen whilst being in my placements, its important that you follow your dreams and goals, and I am looking forward to continuing with mine next year!
Carly Jane Lewis
|
||||||||||||||||||||||||||||||||||||||||||||||
|
This is a report of my first year of the graduate-entry medicine course (GEC), after being very luckily selected for the KMS bursary in 2012. I have lived in the Birmingham/Worcester region for my whole life so far, which is one of the reasons I selected Birmingham medical school. My undergraduate degree was in Biological Sciences, which I studied at Oxford University.
After undertaking a range of work experience activities in a number of hospitals including the QE, Heartlands, Coventry and Rugby and volunteering with a charity that worked with children with learning disabilities during my undergraduate degree I became passionately set on medicine as a career. My last degree had a strong focus on plants and animals rather than human biology, which was a challenge at first. However, the PBL style of teaching that the GEC course offered was very good at accommodating everyone’s strengths and weaknesses. This is because the aim of the summary sessions at the end of the week was to check that everyone was at the same level. During these sessions the problems anyone had were raised and tackled by the whole group. Therefore I never felt like I was behind after the PBL was completed despite my lack of prior knowledge starting the week. That it is not to say it was not a challenging year-because it was! There was a lot of ground to cover in very little time, but that is also what kept it interesting.
I bonded very quickly with the others in my PBL groups, some of whom are now my closest friends. After the first rotation of groups my first group ‘RED group’ would still meet up, and below is a picture of a curry we arranged: On top of PBL teaching I also had a GP placement on Wednesdays in Wolverhampton. This offered a more ‘clinical-feel’ to the year, and was great preparation for the years to come. It also helped on the weeks where I felt overwhelmed with work by providing a break from books.
The summer examinations were hard, but I was extremely pleased and surprised with my results, which was a great end to the year. Come September I am placed at Wolverhampton hospital, predominantly in Cardiology and Care of the elderly. I am really excited for the year ahead, and I hope it will help me get a better-informed idea of what specialties I may be interested in for the future. Before being awarded the KMS bursary I was very worried as to how I would afford the year, in particular the upfront cost of the tuition fees that student finance would not cover. However, because of the bursary I no longer had this worry. It has therefore been a tremendous help in enabling me to undertake medicine as a graduate. I did also decide to keep my Saturday job to help me with living-costs, but because I had won the bursary I was able to take time-off when I needed it for revision for termly ‘reflection exams’ and then for my summer exams without having to worry. On top of the course and my Saturday job I did manage to scrape some free time during which time I managed to make the best of the University, medsoc and the City. Including running the Birmingham half marathon with 3 other GECs for charity, attending the medsoc ball, which was a great night to mix with other medical students from other years as well as some of the professors.
I also took part in the ‘harborne-run’ after our exams, which was a fancy dress evening ran by medsoc. I am the one dressed as cat-women. Overall it was a brilliant, but challenging year. I have gained lots of new skills, made some great friends and I have learnt a lot of medical science in a very short amount of time. Thank you very much KMS for the opportunity to study a second-degree without the financial worry I had coming into the year. I cannot express how much I have appreciated the bursary and how much of a difference it made to my year. Yours sincerely, Heather Bailie
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Vicky La-Borde click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
KMS Bursary Report 2011/12 by Robyn Hill Norwich Medical School, UEA
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
To the Kidderminster Medical Society I am currently on the 4-year graduate entry medicine course at the University of Birmingham. I have lived in various places around the West Midlands all my life. I was born in Solihull, grew up in Birmingham and Sandwell, then later moved to Herefordshire and Worcestershire. Following my passion for the sciences at school I studied Biochemistry at the University of Leeds, and graduated with a first class honours degree in July 2010. After spending most of my undergraduate degree contemplating studying medicine, I spent a very happy year working as a Nursing Auxiliary at Hereford County Hospital on their acute stroke unit, which settled my decision. This past year has been one of the most challenging and enjoyable of my life so far. A whirlwind tour through anatomy, physiology, sociology and all the other aspects of pre-clinical medicine and here I am now nervously awaiting my exam results - I can't believe it has gone so fast! The transition from learning on a lecture-based course to a mostly self-directed course was very tough, and it is impossible not to miss being spoon-fed at times. However, I am confident that the problem-based learning approach employed at Birmingham will stand us in excellent stead for our future careers. My favourite parts of this year have been those that I spent on placement at my GP surgery in Aldridge, Walsall. It was a real pleasure to spend time talking to patients and taking my first steps to becoming a medical professional. As for the future, I have little idea where I would like to specialise, but I am looking forward to working in various areas throughout my clinical years. My first placement is at Heartlands Hospital where I will be based on the Elderly Care Assessment Unit, and I can’t wait to start. I would like to say thank you very much and express my sincere gratitude for being selected as the recipient of your bursary during this academic year. It has been invaluable in relieving the financial pressure of studying a second degree and has allowed me to dedicate more time to studying than would otherwise have been possible. |
||||||||||||||||||||||||||||||||||||||||||||||
|
Lara Reilly
|
||||||||||||||||||||||||||||||||||||||||||||||
|
ELECTIVE REPORT LAURA EASTON
I spent my first three weeks of elective on the male general medical ward in the large tertiary government run hospital in Kandy, Sri Lanka’s second largest city. The ward had over 50 beds and was run by a team of 7 doctors, with consultant-led ward-rounds every morning. Also on the ward were 16 final year Sri Lankan medical students.
My placement objectives were to develop an understanding of the Sri Lankan attitudes towards medicine from the perspectives of both medical staff and their patients, and to therefore develop an understanding of the practical consequences, and to experience the delivery of healthcare in a financially challenged setting. I was enthusiastically welcomed by the medical team and local students, and I spent the majority of my time shadowing doctors on the ward rounds, from which I became familiar with tropical diseases such as cholera and malaria. There were interesting cases such as elephantitis and I was able to regularly examine patients. There were significant differences between UK and Sri Lankan medical provision - the ward and equipment were much more basic, there was no isolation for patients with infectious diseases, and ANTT did not really feature. As patients presented much later than they would do in the UK, this automatically made the doctors jobs more difficult as the patients were more acutely unwell, whereas in the UK they would have been treated well before that stage. Despite this, the standard of medical care provided for patients was relatively high, and I think this was because of the effective team work between all levels of doctors and nurses. The medical students also had far greater freedom than here in the UK and often seemed to take over the ward! I spent my last week in Sri Lanka in a remote village called Habarana where I experienced traditional Aruveydic medicine which involves practices such as herbal drinks and ointments, and various massage techniques, often involving spices as a form of healing over conventional Western medicine. The hospital consisted of an inpatient ward with roughly 5 or 6 patients, and also had daily clinics where anyone could drop in and see the doctor who lived on site. It was very interesting to see a form of medicine I had no previous experience of, and mixing remedies in huge old cauldrons was certainly a new experience!
Outside of placement I was able to enjoy the idyllic beaches of Sri Lanka, buy tea fresh from the plantations, and take part in the pilgrimage to Adam’s Peak which involved an overnight mountain ascent.
I then spent my last month of elective based in the government-run hospital of Western Regional, in Pokhara, Nepal. The Obstetrics and Gynaecology department is the second largest in Nepal, and sees over 30 births as standard each day. My role was to observe and help out on ward rounds, and to assist in the delivery room. The standard of care was very basic, often with 8 women in the first stages of labour all in one room with no curtains between them. When the baby was crowning the women had to walk down a corridor into the delivery room and up some steps onto the delivery bed. The delivery room had 4 beds, again with no curtains between them, and the room was incredibly basic.
During labour all women received oxytocin to speed the process up, and during my time there I saw no-one receive any pain relief, even during episiotomies. Caesarean sections were scheduled for Sunday and Wednesday mornings only, although in the event of an emergency a space in the surgery could be given. I learnt that only 20% of Nepalese women give birth in hospital, and this statistic is trying to be bettered by a government run programme called ‘Safe Motherhood’ set up in June 2010. The programme encourages Nepalese women to attend antenatal classes, and to give birth in hospital. For doing so, and after attending all the antenatal classes and having given birth, the woman receives 1000 rupees (approximately £8). The consultant told me that this programme has been an initial success, and I was encouraged that such a programme existed. I spent my final week in Nepal in a remote mountain village called Nalma, where I worked at the local rural health post. The health post was set up by the government and is run by two workers in the village, one a mid wife, and another with limited healthcare experience. The post has a limited supply of drugs including antibiotics, iron supplementations, oral rehydration sachets etc. The post is open every weekday from 10am-3pm, during which time anyone can drop in and be seen. During my time I saw wounds that needed to be dressed, common coughs and colds, gastroenteritis and alcoholism. The post also offered a family planning service and I was able to administer depo vera injections. The post is able to refer patients on to hospitals and is an invaluable first stop for locals who would otherwise not be treated for minor ailments or who would have to walk for hours to get to the nearest hospital.
Nepal is an amazing country, and I was lucky enough to experience Holi,the annual festival of colour which saw us being covered in paint by locals, as well as enjoying several treks in the Himalayas, the highlight of which was watching sunrise on the top of Poon Hill after a hard three day ascent!
Laura Easton
|
||||||||||||||||||||||||||||||||||||||||||||||
|
From the West to Wewak: A Medical Student's elective in Papua New Guinea Aim To explore healthcare and its delivery in a lesser economically developed country; drawing comparisons with the NHS with the intention of trying to shape our services for the better on my return. Objectives of the Project i) To become emersed in the medical culture of Papua New Guinea, exploring beliefs, behaviours and attitudes towards health in a population very different from our own. ii) To see how specific groups of people in Papua New Guinea interact with healthcare services: specifically women, the elderly and people living with chonric diseases. iii) To learn more about tropical diseases and H.I.V. from patients and professionals from a experiential point of view iv) To consider how the delivery of healthcare may be tailored to a more economically strained setting and how money (or the lack of it) effects healthcare provision in Papua New Guinea. Explain how you achieved the aims and objectives of your elective. Objective 1: I sought out patients from the groups I was considering and kept anonymous records of their management/presentations etc. I contrasted the patient's treatments to those in the UK, in my reflective journal. Objective 2: Each day I have seen cases of malaria in addition to TB, HIV, leprosy, tropical splenomegaly, worms etc. I have learned their presentations/managements and have made a portfolio of interesting cases. Objective 3: The lack of resources available was evident: e.g. the hospital lacked a water supply most days. Each evening I reflected on how the staff dealt with such dilemmas in my journal.
Were there any flaws in the methods you used to address your aims and objectives? Describe them. If none, explain why you think there were not any? On arrival, I discovered that the hospital had been hit by a tsunami caused by the Japanese earthquake. Hospital services had been reduced to cater only for emergencies. Accordingly I modified the planned methods for my objectives to take this into account. E.g. for Objective 1, I had to examine how patients presenting with acute complications of chronic disease usually managed their disease, rather than attending their routine clinics etc. 'Flaws' in my planned methods were circumstantial rather than due to problems with my preparation and I overcame them by adapting my methods within the scope of broad objectives.
What were the Learning Outcomes from this elective? Were they what you expected? During my elective I feel that I have met each of my planned learning objectives but the stark nature of some of the patient's conditions and circumstances has left a deeper emotional stamp on my memory than the intellectual exercise I wished to achieve. It is one thing, for example, to want to understand how women interact with healthcare services in a developing country but it is very much another to be confronted by a woman in A&E who has suffered domestic abuse at the hand of her machete wielding husband whose only punishment would be a set hospital fine (6 pounds sterling). Reflect on how your Elective complimented your medical undergraduate career (a deeper understanding of life; a better understanding of communicable diseases; etc.) Has it affected your future career intentions?
On reflection I realise that I have been able to develop many of the skills that have been fostered during my undergraduate training whilst studying in PNG; procedural skills, consultation frameworks, advanced communication techniques with non English speakers etc. These experiences will have direct practical value for my foundation training.
However, I now feel that other, less tangible, aspects of my study here will have a greater effect on me as a doctor going forward. I have witnessed the great social and physical impact of chronic disease on people who receive little treatment, been exposed to deaths from diseases I consider easily preventable, and seen the serious social stigma that people can receive due to illness and much more. These experiences have given me a greater understanding of what it is to be a patient, the patient's narrative. These are valuable insights that will remain with me forever and will improve my future practice.
My time in PNG has
given me much exposure to infectious disease medicine and has
perpetuated my desire for a career in this field. Having seen the
importance of infectious disease prevention here, I am now strongly
considering applying to spend some time at the W.H.O. Would you recommend this location to another student? Why?
In PNG I have learnt not only about tropical disease, trauma etc. but also the art of practising medicine where resources are scare and poverty is abundant. All whilst bathed in the tropical sunshine of an island with some of the warmest people I've met. I would absolutely recommend it.
Daniel Cox
|
.jpg) The Cholera Unit following the Japanese Tsunami
Medical Records following the Japanese Tsunami
The Hospital Kitchen
The Pharmacy following the Japanese Tsunami
|
|||||||||||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Elective in Australia |
||||||||||||||||||||||||||||||||||||||||||||||
|
I spent my elective in Australia; one month in a GP practice near Brisbane and one month in The Royal Darwin Hospital in the Northern Territory. My GP placement helped me to develop my history and examination skills and because of the high incidence of skin cancers in Australia I was able to assist with many excisions and improve my suturing. There were many similarities to general practice in the UK but significant differences in the way the healthcare system is funded, which was very interesting. I also came into contact with conditions I hadn’t seen before; scarlet fever, Giardia from water tanks and Rickettsia from tick bites. One patient brought in a funnel web spider that had bitten her but luckily there was no venom released! Being in Darwin was a very different experience and was very interesting. A WHO report states that there is a 20 year gap in the average life expectancy of an Australian and an Aboriginal person.1 I was with the Renal medicine team and saw the problems associated with the large area the hospital is trying to cover; the Northern Territory is six times the size of the UK with only five hospitals. The hospital runs outreach clinics to improve healthcare access for aboriginal people living in remote communities and I was able to attend one of these on the beautiful Tiwi Islands. Through talking to doctors and patients I was able to learn a little about Aboriginal culture and can appreciate some of the differences from Western society. This elective was fantastic and I learnt about renal medicine, the challenges faced in providing access to healthcare over a large area, and working with patients who have differences in culture and health beliefs. I was very lucky to have this experience and greatly appreciate the bursary from the Kidderminster Medical Society that helped me go on my elective Thank you! Harriet Webb |
||||||||||||||||||||||||||||||||||||||||||||||
|
click to go to Index at top of pa
|
||||||||||||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Year 1 Bursary Report
|
.jpg) |
|||||||||||||||||||||||||||||||||||||||||||||
|
Hello, I’m Robyn Hill and you very kindly awarded me the KMS bursary last year. I’d like to take this opportunity tot hank you and show you a snippet of my life as a medical student at Norwich Medical School , UEA .
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Curriculum UEA is problem-based learning (PBL), systems organised, 5-yr MBBS. On Friday mornings, in groups of 10, we meet with out PBL tutor and go over the week's scenario. From this we produce learning outcomes for the next week. These are divided between the group members (each having 2) and the work is due in on coming Tuesday. The timetable was the same each week. Monday's lectures and anatomy, Tuesday lectures and seminars, Wednesday is a half day with anatomy and inter-professional learning in the morning, Thursday is GP placement and Friday is PBL with presentations of our learning outcomes and brainstorming for the next week. The last lecture of the day on Friday is "wrap up". A consultant or GP will come in and go over the key topics from the week. Hospital placement This year I have had 2 hospital placements both at the Norfolk and Norwich University Hospital. In the New Year I was in oncology for 4 weeks and in the summer I had another 4 weeks in rheumatology and orthopaedics. Oncology was not at all what I expected it to be and the consultants gave me a different view of cancer. They highlighted that for patients with chronic illnesses such as respiratory problems, often there is limited amount doctors can do. With cancer patients some can be successfully treated and for many people years can be added on their lives. The rheumatology and orthopaedic placement was more hands on- including a rememberable paediatric session with 10 children aging from 0-15yrs. In groups of three we had ten minutes to get a history, examine and then diagnose the child before moving on to the next child. It finished up with the group having to present the case to the consultant surgeon to show what we had found out. Theatre I was lucky enough to go into theatre when I was on my oncology rotation and saw open chest surgery. The surgeon even let me scrub up and assist him (he let me cut the thread which was very close to the heart!). I also had surgery slots for orthopaedics and saw hip replacements, shoulder arthroscopy, a compartment syndrome patient and time with the anaesthetist prior to surgery. The anaesthetist was particularly nice and once they had given the anaesthetic they let me do the breathing for the patient by squeezing the air bag and during the long operation taught me basic life support for my forthcoming OSCE (I achieved full marks for BSL which I give much credit to the anaethetist!). GP Placement I spent each Thursday in general practice at Stowmarket Surgery in Suffolk. It is a very large practice including it's own gym and alternative medicines shop. We had 2 GP tutors Dr. Rebecca Ball and Dr. Cort Williamson - one for the morning and one for the afternoon. In pairs we saw patients twice a day for an hour where we practiced history taking, taking manual BP and practiced examinations. The rest of the time was spent with the tutors, learning new examinations, drugs of the week, prescribing tasks and using the clinical system to get data on patients for our logbooks. Anatomy Dissection places at university are limited due to the small size of the dissecting room however I managed to get a place on it next year. I am looking forward to this but apprehensive as it dramatically increases your workload as we teach the non-dissecting students in addition to the actual dissection time. |
||||||||||||||||||||||||||||||||||||||||||||||
|
I lived in university halls, Beech Flat (picture above) and made some lovely friends. The six medical students in the flat got on so well that we have decided to live together next year. 5 of us are graduates and one 18-yr old proper fresher. I am pleased to report that I successfully past my
exams and will moving onto the second year in September.
The year is banded A-D and tantalizingly I was 1 mark off the top band in my autumn exams and 2 marks off the top in my summer exams. I am happy I passed well but next year my aim is to be in the A band and then in the final three years move towards a distinction. I am already looking ahead to my elective and particularly interested in the opportunity of spending it at Yale University. International students are eligible to do 2,4-week placements alongside the Yale students at local hospitals in America. When I moved to Norwich I joined the university rowing club and trained with the women's squad. I did a little bit of coxing and rowing. Unfortunately, Women's Henley fell on the week of my exams and 8 sessions of training proved hard manage with medicine. Instead I started running and currently considering entering the Edinburgh Marathon with couple of the other students. Now I'm settled into medical school I would like to go back to rowing. The UEA medical students have a reputation for fancy dress and by the end of the first year I had been a surgeon, Frankenstein, a Fantastic Four and Harry Potter's Professor Trelawney........
|
||||||||||||||||||||||||||||||||||||||||||||||
|
As soon as term ended I returned home to Bewdley and began working at Upton Surgery, Worcestershire summarising medical notes and doing clinical audits for them. I am currently working 40hrs a week and saving money towards my living costs and the first term fees for next year. I am hoping to take to have a few days off before returning to Norwich, so I can have a break before term starts in September. Finally Once again I would like to thank you for the generous £3000 bursary. It enabled me to focus on my studies rather than constantly worrying about how to pay my fees. I cannot thank you enough for this. Leaving my job, moving away from my long-term boyfriend and family to the other side of the country was hard and the financial pressure being reduced for the first year made this difficult time a lot easier. I have thoroughly enjoyed medicine and feel that I made the right decision. I have made some lovely friends and looking forward to next year - dermatology, haematology, respiratory medicine and cardiology. I think it will be a very busy year!
Robyn Hill
|
||||||||||||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||||||||||||
|
An Elective in Masaka, Uganda James Parsons, 5th Year Medical Student, University of Birmingham
In April earlier this year I embarked upon my medical elective as part of the MB ChB programme at the University of Birmingham. I decided to travel to Kitovu Hospital, a small missionary led hospital in Masaka, Uganda. The focal point of my project was to look at the diagnosis and management of HIV and Malaria. I chose to go to Uganda as these two diseases are the two biggest contributors in terms of mortality of the population.1 Along with this I wanted to get a comprehensive experience of what healthcare systems are really like in third world countries, where resources are often scarce and simple diagnostic tests are often unavailable. I therefore spent each week of my four week placement rotating between the four main wards in the hospital: Medicine, Surgery, Obstetrics & Gynaecology and Paediatrics. During my first week I shadowed and assisted the hospital physician on the medical ward. This entailed daily morning ward rounds followed by ward jobs, procedures and medical outpatient clinics. HIV and malaria are common conditions. At any one point at least half of the ward (15 beds in total) were being treated for Malaria. These patients would often have massive hepatosplenomegaly and so I was able to practice and improve my examination skills to great effect. This week also allowed me to see first hand the difficulties faced by doctors in the third world. During the week I was on the medical ward the radiographer was on holiday and so there was no imaging modality available at the hospital. Instead doctors would either have to send patients to the next large hospital to have an x-ray, which would often take days, or rely purely on clinical signs. This helped me to truly appreciate how lucky we are to have access to such comprehensive healthcare here in the UK. Following this week I spent a week on the Paediatrics ward, which was coupled with both the Hospital Nutrition Unit and the Hospital Outreach Team. During this week I helped manage the 30 young children on the ward. I have yet to do Paediatrics as a specialty in the UK and so this gave me a brilliant opportunity to learn about the different problems children experience and also to learn how to go about examining a child.
As stated above I also got to spend some time on
the Nutrition Unit where I was able to see numerous children with
Marasmus and Kwashiorkor. I was shocked at how poor some of the
families were. The parents often didn’t even have enough money to
feed themselves, let alone their children. |
||||||||||||||||||||||||||||||||||||||||||||||
|
My final two weeks were spent on the Obstetrics & Gynaecology ward and the Surgical ward. My week on the Obstetrics & Gynaecology ward allowed me to develop my confidence in dealing with and managing a pregnancy. I also got to watch and assist surgeons carrying out Caesarian sections, which was an extraordinary experience, as again I have yet to do my Obstetrics placement in the UK. The week I spent on the surgical ward was also just as rewarding. I was allowed to practice my suturing skills a number of times and I also watched several emergency operations being carried out. Overall my elective was a challenging but incredibly rewarding experience and I would like to thank the Kidderminster Medical Society for the bursary they provided me with to help fund it.
James Parsons
|
||||||||||||||||||||||||||||||||||||||||||||||
|
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||||||||||||
|
A year in Natal
Thomas Mendes da Costa KMS Bursary 2009/10 MSc Trauma Surgery
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Again I would like to express my appreciation for the bursary from the Kidderminster Medical Society which, despite the title of this article which will become apparent shortly, was used towards funding my recently completed Masters degree in Trauma Surgery from the University of Wales. Many reading this will I’m sure know my father Dr Baron Mendes da Costa, who worked as a local GP in Kidderminster for 30 years until his retirement early last year which I can assure you has done little to slow him down! Although following the same degree path, we have deviated widely in specialty, and I am currently in my third year as a registrar of Orthopedics and Trauma in the Severn Deanery. Whilst in the twilight of my career I am sure a quiet elective list of a bunion or two and the occasional arthroplasty will be quite fulfilling, my interest during junior surgical training has always been traumatology. It is this interest which has led me on to the Masters degree course run at Morriston Hospital, Swansea. The trauma unit at Morriston Hospital is currently one of the few in the UK to offer all specialties required to support poly-traumatised patients on site, most centres requiring referral links to specialist centres as a patients needs dictate. This includes burns, plastics, vascular and neurosurgical teams to support the surgical, orthopaedic and intensive care teams who make up the front line trauma response team. This provided an ideal setting and a wealth of experience form which a years taught course programme was formulated, concentrating initially on the physiology of the traumatic process, kinetics of trauma, and the indication and effect of early resuscitative or emergency intervention, through to methods and timing of emergency and definitive surgery, and culminating in recovery and rehabilitation. Visiting military and civilian lecturers covered the broad range of challenges posed by the spectrum of both trauma and the individuals affected, with real time scenarios played out with (sometimes all-to-realistic) medical actors to ensure the practical and theoretical elements to trauma care were all addressed. Following the taught course, a dissertation was undertaken, for which I studied open fractures of the tibia. If you will excuse the dramatism, this is essentially a broken shin bone sticking out the skin and the decision of exactly what to do with it. Treatment of the complex fracture patterns, with associated commonly severe soft tissue injuries, can be a difficult decision for patient and surgeon alike, as treatment varies from fixation and closure to amputation, with multiple options in between. These include a variety of fixation methods (plates, intramedullary nails and external fixators) and requirements for treatment of surrounding soft tissues (debridement, need for plastic surgical flap coverage etc). To assist the surgeon with this dilemma there are a number of scoring systems that are used on presentation to help guide treatment and prognosis, so as to select the best method for salvage and rehabilitation, whilst not exposing the patient to the risks of lengthy salvage operations which may increase the risk of morbidity or mortality without yielding a superior result. My study focussed on comparing one new and one mainstream scoring system with the well established system already internationally used but widely regarded as being of little practical use. These scoring systems would be used on all patients presenting with open tibial fractures, and the eventual outcome compared to the recommendation of each system.
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Open fractures of the tibia are thankfully a relatively rare injury in the UK, making it an unsuitable location for this study. An area with much higher incidence of trauma was needed. Ngwelezane Hospital, in a township outside Empangeni in rural Kwazulu-Natal, South Africa, provides a tertiary referral service for trauma throughout the northern third of Natal, some 2 million people. Run by an ex-pat consultant from Sheffield and with a mix of Black African, Africaans and Western doctors, the hospital workload consists of high levels of interpersonal assaults, violent trauma and motor vehicle accidents, amid the epidemic of HIV and TB. This would be not only the ideal setting for dissertation data, but would provide an incredible training experience in the management of types of trauma usually uncommon and treated by senior surgeons in the UK.
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Having obtained deanery and college approval, I commenced work as a medical officer in February 2010. The Orthopaedic department was extremely busy, and, along with a thankfully never-ending supply of nurse translators, and surprisingly patient locals who would think nothing of a four plus hour wait to see the doctor, the long queues of patients in chairs and on stretchers were tended to three times a week. Three all-day trauma lists ran side-by-side twice weekly to fix those who could wait, and a non-stop trauma list was available for the operative emergencies. Surgical instruments and implants were in good supply, but the pressures of blood shortages and periodic civil strike action were new challenges to face. Seniority was achieved quickly working in this environment, with surgical skills acquired being taught in turn to those more junior to enhance the strength of the available workforce.
|
||||||||||||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||||||||||||
|
The levels and type of trauma was formidable. Gunshot and panga (African Bushknife) wounds were commonplace, with accidents involving overcrowded and poorly maintained vehicles often resulting in multiple severely injured casualties. Whilst I thankfully survived the year suffering nothing more that minor theft, the high walls, electric fences and numerous security companies offering armed response units at the press of a button bore testament to the perceived levels of danger in the area. This was soon a part of everyday life and certainly with the excitement of the FIFA world cup being hosted in South Africa (which anecdotally dramatically cut trauma rates), Natal was one of the most beautiful and culturally diverse places I have visited. The warm Indian Ocean, the spectacular Drakensburg mountains and multiple reserves sporting the big 5 were simply breathtaking. Be it vineyards in Stellenbosch, shark diving on the south coast or the beauty and cultural diversity of Natal, South Africa really does have it all!
|
||||||||||||||||||||||||||||||||||||||||||||||
|
During my eleven months in Africa, I succeeded in following up twenty patients with open tibial fractures to gain the data for my study which provided statistically significant evidence that their application can predict outcome and guide treatment. These systems were adopted in Ngwelezane Hospital following the study. Dissertation results from the university are pending and will be followed up by submission to publication in the international orthopaedic literature.
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Ostrich farm, Oudtshoorn, Western Cape, South Africa
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Kidderminster Medical Society Bursary 2009 A report from Gemma Plant who was last year's recipient at Birmingham University Medical School. I am writing to express my sincere gratitude to the society for the Bursary awarded to me in 2009. This has provided me with invaluable financial support during my first year of the Graduate Entry Course (GEC) at the University of Birmingham Medical School. The money awarded by the Society made a significant contribution to my tuition fees for the year and helped massively to ease the financial burden of my return to student life after four years of full-time work. I graduated from The University of Birmingham in 2005 with First Class Honours Degree in Biological Sciences, and then worked in Pharmaceutical Sales until returning to University last year. I have always been interested in Medicine but my desire to become a doctor grew significantly as a result of exposure to the profession in my role as a Medical Representative. The decision to return to university was a difficult one, since it involved many sacrifices. Before applying to university I felt I should gain direct experience of medicine. To do so I acted as a volunteer at Mary Steven Hospice, and I shadowed a number of doctors in both general practice and hospital. I was aware that there is significant competition for places on graduate courses and was delighted when I was offered a place to study medicine. The first year of the graduate course was very intense, involving study of what is normally two years worth of pre-clinical theory in nine months. Much of the learning process was “self taught” with the majority of the material in the year being predominantly based on problem based learning (PBL). Overall I had a great year and found the work challenging but importantly interesting and rewarding. I have made some wonderful friends amongst my peers, since we depended upon one another for support as we progressed through the PBL modules. The learning process and experience was fantastic and has increased my passion to enter the medical profession. Having successfully passed the initial year, I have now joined the third year of the Undergraduate course and am currently on my first clinical placement at Walsall Manor Hospital. This is an integrated medicine and surgery placement and I have already seen many interesting cases and learnt many new skills. Although the first few weeks in a hospital setting were daunting I love every minute of the experience and can honestly say I have never regretted my decision to return to study medicine. I will remain forever grateful and indebted to Kidderminster Medical Society for being a part of making it possible. I had the pleasure of attending your annual dinner last month with one of my GEC colleagues. Both Julia and I had a lovely evening and very much appreciated being invited and made to feel so welcome. Hopefully I will have the opportunity to train or work in the Kidderminster area and in some small way be able to repay the investment the society has made in my career. Once again, my sincerest thanks for you support and commitment to me. With all best wishes to the society and its members, Gemma Plant
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Medical Elective Report
Kimberley Eaton Charnock 30th June 2010 For my medical elective I chose to go to Tanzania, Africa. The main reason for this was because I thought going to a third world country would give me great insight into working with few resources, being challenging as well as experiencing a completely different culture. I went to a large government hospital called, Mount Meru District hospital in Arusha, (Northern Tanzania) where I worked in obstetrics, general medicine and casualty/outpatient department. I also went to a remote Maasai village where I spent a week at a dispensary, similar to a general practitioner (GP). In the obstetrics department I spent time learning from the staff, made up of doctors and nurses who were experienced in assisting childbirth. The delivery suite was an open 20 bedded ward, where all enter, were assessed and gave birth. So you could see all stages of labour simultaneously. Whilst I was there I assisted in vaginal deliveries, a breech delivery, neonatal resuscitation, watched caesarean sections and went on the daily ward rounds for all obstetric and gynae patients. This experience enabled me to develop my own confidence in delivery babies naturally, particularly as there was no analgesia. The general medical ward was made up of all medical specialities. There were a total of 60 beds, half female, half male. But when the beds were full there would be more than one person to a bed, sometimes this made it difficult to examine patients properly. Often patients had infectious diseases such as gastro-enteritis/pneumonia and were sharing beds, which was obviously not ideal. I learnt how to treat diseases that are not common in the United Kingdom (UK), such as malaria and HIV as well as how common diseases such as pneumonia and asthma are treated in a third world country where there are no oxygen facilities. Here I worked with the Intern doctors (foundation year doctor equivalent), which was very good because we compared our education and learnt a lot from each other. I found there were limited investigation services available in the hospital, and even if a doctor ordered an investigation it was often not carried out due to demand, or no availability. There was no CT or MRI scanner and only one ultrasound and X-ray facility so actually getting a patient to receive this was rare, compared to UK. Anti-biotics were often unnecessarily used or multi anti-biotics were used, doctors were aware they were over-using antibiotics but said it was due to lack of availability of investigations, such as sputum sample culture and therefore it was better to give many broad-spectrum antibiotics. I think this will be a much bigger problem in the future, particularly in those with HIV. I saw quite a few diseases there which I will probably never see in the UK, such as a death from Pellgra, a vitamin deficiency. I spent one week with a remote large Maasai tribe, where the population was about 4,000-6,000 people. During this week I went to the dispensary daily, where I worked with a doctor and a nurse. This was very similar to a general practitioner (GP). We would see patients on a first come first see basis. Patients often travelled from far away. I was surprised how many patients came with similar problems to the UK, such as head and back pain, muscle spasm etc. The doctor also ran an antenatal clinic one afternoon, a current topic of improvement in Tanzanian, where they are trying to reduce maternal and baby mortality. This week was very enjoyable, where I learnt about tribal life, Maasai culture, all helped by living with them, and I also met the local “medicine/spiritual” healer man. He still sees a lot of patients for a variety of bodily and mental complaints, however the popularity is reducing with the availability of modern medicines and the ever-popular anti-biotic! I spent my last week in the casualty/outpatient department. As there are no GPs in Tanzania, all patients present to the outpatient or casualty department and are seen on first come first seen basis. This was a busy week, with many patients of every speciality including follow-up patients. It is from this department that people are admitted from the hospital too. I thoroughly enjoyed my time in Tanzania and am eternally grateful for support I gained before going. All this made it possible for me to go. I learnt many things about the difference in healthcare worldwide and the importance of team work and a variety of education amongst health care workers, and just how lucky we are in England to have the NHS team. Kimberley Eaton-Charnock
|
||||||||||||||||||||||||||||||||||||||||||||||
|
An Elective In Zanzibar Amy Mountain - 5th Year Medical Student-Keele University I chose to undertake my medical elective in Zanzibar, a beautiful tropical island off the east coast of Tanzania. The hospital where I worked was called Mnazi Mmoja, the only government run hospital on the Island serving a population of 1 million people. The hospital is evidently deprived of resources-yet the staff utilise what they do have incredibly well. I was shocked to learn that the only source of oxygen was in the intensive care unit. Patients also have to pay for all interventions, medications and investigations. Prices ranged from 75 pence for a full blood count to 15 pounds for an above knee amputation. This was all very expensive for patients who try to avoid going to hospital and will seek ‘local remedies’ in the villages instead. I spent 4 weeks on the female medical ward as well as time in the eye hospital, paediatrics and psychiatry. Experience in so many specialities was great and so were the staff. Common day to day presentations included malaria, diabetes, hypertension, anaemia (which was incredibly prevalent), complications of human immunodeficiency virus and diarrhoea. One of the most shocking sights was when patients had severe diarrhoea. If they were very weak they would be placed on a bed with the mattress folded in half. This ensured that when they defaecated their faeces fell through the rusty metal springs of the bed into a bucket below. No attempts were made to preserve the patients’ dignity. There were many cases of cholera during our time there, possibly due to a 3 month power cut that affected the water supply. A big learning curve for me was that resources were simply not available to perform multiple investigations and seek out a diagnosis as we do in the UK. This often meant many patients were discharged without a diagnosis. At first I found this frustrating but it did highlight how fortunate we are in the NHS to have a battery of tests at our fingertips and this is probably taken for granted at times. I learned a great deal from this experience and I would like to thank the Kidderminster Medical Society for the bursary towards my elective. It made my elective an even more enjoyable experience and one I shall never forget!
Amy Mountain
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Helen Dale Report as a GEC 1 at Birmingham University. Recipient of KMS Bursary I started my first week at Birmingham University as a graduate entry medical student with a mixture of trepidation and excitement for the forthcoming year. I had been told that the first year of the graduate entry course (GEC) was very work intensive, and required high levels of self-motivation and group-working skills necessary for the self-directed learning component of the course. It seemed like a very ambitious task to learn the equivalent of the first two years of the undergraduate medical course in one year, but having made it through the year, I can tell you that it is possible! The first year of the GEC course is predominantly 'taught' by PBL (problem based learning). This involves working in small groups (8-9 students) in rooms at the medical school. Each week we were given a clinical scenario: about half a page of a history of a patient. From this scenario, we would as a group, run through the following process: - Define any terms we were not familiar with. - From this, we tried to put our ideas into order and make links between topic areas. - Create learning objectives based on the topics we felt we needed to cover that week. - Go away and learn independently the topics identified in the learning objectives. - Meet up again later in the week, and discuss what we learnt and identified areas we didn't understand well. - From the areas we didn't understand, create questions to ask an expert panel for clarification. The course was divided into six blocks; cells and cancer, cardiovascular and respiratory systems, neuroscience, gastrointestinal and urinary systems and metabolism, reproduction, and infection and immunology. Each block consisted of three to four PBL scenarios. We also had supplementary lectures during the week, which covered areas related to the scenario that week, and three hour anatomy tutorials with an anatomy demonstrator. The anatomy teaching was supplemented by a prosectorium visit every four weeks. This was invaluable for consolidating our anatomy knowledge and understanding how the two-dimensional images in the textbooks related to actual three-dimensional bodies. Our clinical experience consisted of a day at a General Practice Surgery every week. I was based in Riverbrook Practice in Stirchley. This provided us with a break from the textbooks, and a chance to see how the diseases we were studying affected individuals in their day to day lives. It was a great opportunity to develop our communication and history taking skills, by talking to patients, and also a chance to practice clinical examination skills. I personally found this day to be the most enjoyable, and a time when it was possible to see how the theoretical work was practically applied to treat patients. During the first month of the course we had the opportunity to complete a Basic Life Support (BLS) course. This took place on Monday evenings, which consisted of four sessions with an assessment at the end. I really enjoyed this course as it allowed me to develop some practical skills. Outside of the academic work, I became involved in the University Mountaineering Club. I went on a number of climbing trips, including a winter mountaineering trip to the Cairngorms over the new year, trips to Wales and the Peak District, and a trip to Fontainbleau in France at Easter. I also joined a running club and the medics swimming club. Overall, the GEC students were a very friendly group and we got to know each other well throughout the year. Despite the intensity of the course, I did enjoy it and learnt a great deal which has put me in good stead for clinical work this year, and in the future. I would like to thank Kidderminster Medical Society for the bursary that they awarded me; it certainly made life easier for me during this year and meant that I could focus wholly on my studies without unduly worrying about the financial pressures of becoming a student again. I am also extremely grateful to the Society for inviting me to the Annual Dinner and for making me feel so welcome. Many thanks, Helen Dale
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Katie Levitt An elective in the Caribbean, an experience of healthcare in two developing countries
Details of Venues and health and safety: I spent a month at St Ann’s Bay Hospital, Jamaica and a month in Victoria Hospital, St Lucia. My supervisors at the institutions were: Jamaica
Dr Horace Betton St Lucia
Dr Elisabeth Lewis Main Report: Aims and Objectives The main aim of my elective was to experience healthcare provision in two developing countries. I wanted to contrast the healthcare provision, practice and attitudes towards health between the Caribbean and the UK. I was interested to gain the views and beliefs of patients and doctors in a foreign country to broaden my cultural horizons. I was also interested in learning about how healthcare is provided in these countries in contrast to the National health framework used in the UK. Whilst abroad I wanted to challenge myself to learn medicine in an unfamiliar and self directed environment. I felt it very important to learn how to adapt to a new environment whilst continuing my learning; a skill I will need to implement when I begin my foundation year training. I am now going to talk about the month I spent in each country separately, beginning with Jamaica. Jamaica, September 2009
"It is the fairest island eyes have beheld; mountainous and the land
seems to touch the sky” Jamaica is famous for having the most churches per square mile of any other country in the world. Ironically it is also famous for being a violent country, with an estimated 3 murders occurring per day. The official language of Jamaica is English and most correspondences are written in Standard English. However, the Jamaicans have developed their own spoken language, Jamaican Creole or Patois, which is a mixture of African and English. I soon discovered that patois is very different to the English language and would take some getting used to. I had a month to practice the language and learn about the culture in the St Ann’s Bay hospital, St Ann’s Bay where Columbus had landed many years earlier. One of my first experiences in the hospital was that of a paediatric ward round. The paediatric ward, like all of the others, was nothing like the ones in England. They were all free standing buildings with windows without glass but shutters instead to keep the ward cool. Patients were crammed in to available spaces wherever possible, despite the number of curtains. Cleaning staff kept the ward generally clean, but not up to UK standards. Cobwebs were still visible in the corners of the rooms and dust had settled on the windowsills. Despite this all of the patients seemed generally happy and comfortable.
|
||||||||||||||||||||||||||||||||||||||||||||||
|
The first thing I noticed as we began the ward round is that the doctors do not wash their hands after each patient contact. Infection control in the form of hand washing is not as strictly implemented as in the UK. The doctors and ward staff can wear rings, watches and long shirts to work in; items banned in the UK due to the bare below the elbows policy. The doctors did not seem aware that the practice of hand washing was important in reducing the spread of infection. In the UK hand washing is so highly publicised and now the cultural norm. I assumed that the same practices would occur all over the world, based on clinical evidence. It was reported by the National Audit Office that hospital acquired infections could be reduced by 15% with correct hand hygiene (2). The lack of hand washing could be attributable to shortages or lack of cleaning products in the country. This has been identified by a paper looking at infection control globally. The table opposite shows just some of the problems that developing countries like Jamaica face relating to the implementation of infection control practices. The paper suggests that developing countries may be aware of the practice of infection control but do not have access to the training or funding to implement this practice (3). When I asked doctors about hand washing they were all familiar with the practice but were not strictly told to implement it. This experience, although a surprise, has shown me that healthcare is affected by many factors; money, culture and evidence based best practice are some of these. I was beginning to understand some of the difficulties and barriers that developing countries face to provide good healthcare. The second thing that caught my attention on the ward round was the doctors’ lack of communication. It was the norm to stand around the end of the patient’s bed and talk about their history and condition without involving them in the conversation. This was often done without a curtain drawn around the bed, even when a physical examination was conducted. Usually once a management plan had been decided upon the doctor would communicate this to the patient or parent very bluntly and then move on. I found this lack of communication unsettling. From our first day of clinical practice we have had the skill of communication put at the centre of becoming a great doctor. Poor communication may be part of the culture in Jamaica, but it is very upsetting to observe. This experience has taught me the value of effective communication. I believe that the patient should always be fully informed, involved with decision making and respected as an individual and will always implement these when dealing with patients in the future The St Ann’s Bay hospital is a Government run establishment. Despite this service users have to pay fees to the hospital for all medications, specialised investigations and for transportation, including an ambulance service. A ‘friends of the hospital’ group arrange fundraising events to raise money for the hospital to help subsidise the cost of care for those who cannot afford it. The experience of this provision of healthcare has made me appreciate the greatness of the UK’s ‘free’ National Health Service. All who require healthcare in the UK have access to it, unlike in Jamaica where if you cannot afford to pay you do not receive the care. |
|
|||||||||||||||||||||||||||||||||||||||||||||
|
|
This was demonstrated whilst on a medical ward round. I met an elderly lady who had been admitted with a suspected stroke. The medical team looking after her wanted to get a CT scan of her head to confirm the pathology and diagnosis. However she had very little money to pay for the scan and her family were unable to help. This meant that the diagnosis was not confirmed by a CT scan and the extent of the damage to her brain remained unknown. There is no doubting that the Jamaican culture is a rich, diverse and dynamic one. Part of the culture involves a very paternalistic idea of healthcare. Doctors are seen as the ones with the medical knowledge and should always know what is best for a patient. Patients trust and respect the doctor’s advice. This is a vast contrast to the UK. We are moving towards a shared doctor-patient relationship, one in which the patients help in the decision making process of healthcare. Most patients in the UK like to be well informed of their medical condition and health and have a say in what is best for them. I was shocked to see this ‘traditional’ model of healthcare and how popular and happy patients were with it. This paternalistic model of healthcare does have its downfalls. Patients are reliant on the doctor to manage their conditions and patient education, a vital component of healthcare, is often missed out. This was demonstrated by the high prevalence of type 2 diabetes in Jamaica; estimated to be 17.9%, the highest out of all the Caribbean islands (4). The Jamaican diet is high in sugars and fats, leading to obesity and the problems related with this. On the surgical wards I saw many patients who had been admitted with the complications of type 2 diabetes. Many had large, infected diabetic ulcers that required debridement. Some were so extensive that it had led to the complete loss of a foot or limb. I was disturbed as to how many patients had these drastic complications of the disease. It seemed that education about medicines and diet had not been successful and patients were unable to manage their own conditions. This experience has taught me just how vital it is that patients gain an understanding of their own health and how to best manage it. As a doctor I will take time to do this for my patients. |
|||||||||||||||||||||||||||||||||||||||||||||
|
St Lucia, October 2009 St Lucia is a smaller Caribbean Island, situated farther South and East of Jamaica. It is part of the British Commonwealth and the Queen still appears on all local currency. Like Jamaica, St Lucian’s are extremely proud of their culture. I was lucky enough to experience Jouen Kweyol (or Creole Day in English) a cultural festival that celebrates the local food and national dress of St Lucia. The official language of St Lucia is English, but the spoken language mixes French, English and African to create a unique patois language. Like Jamaican patois, it was incredibly hard to understand and would require yet more practice in the Victoria Hospital, Castries to learn. The Victoria hospital is a public, government run hospital that serves a population of 100,000 people. It is the larger of two hospitals on the island. At the time I was on placement in St Lucia a fire had swept through St Jude’s, the other public hospital on the island, which meant that the workload had considerably increased for all of the staff at Victoria. Although the hospital was a public one all patients that visited had to be covered by health insurance to pay for the costs, much like the system in the United States. A doctor explained to me how it was very common practice for a patient to provide the incorrect contact details so that they cannot be traced after leaving the hospital. The Government then clear the cost on behalf of that patient. This is a new way of cheating the healthcare system in the country that is becoming more popular with residents who cannot afford medical treatment. My chosen rotation in this hospital was gynaecology. As part of the gynaecology rotation I spent a morning in surgery. There were two operating theatres in the hospital; one was specifically designated to obstetrics and gynaecology cases. There was a small recovery area between the two operating theatres and a corridor outside the theatre that was used as the waiting area. The operating theatres themselves looked out onto the Castries harbour with spectacular views. They were well equipped with the necessary modern technology, as used in England, but they did lack the laminar air flow mechanism which prevents the settling of organisms in the operating theatre and reduces post-operative wound infection (5). I observed a caesarean section in surgery. The one thing about this operation that I will always remember is the poor communication with the patient. This lady was visibly distressed and anxious whilst waiting outside the operating theatre and at no point did any member of staff reassure her that everything would be ok. This was displayed again when the anaesthetist was speaking over the patient whilst she was being cleaned and draped for the procedure. It would seem that this is the culture in this country; one similar to Jamaica. Poor communication was demonstrated time and again whilst on ward rounds in the hospital. As a future doctor I feel that keeping the patient central to care and maintaining their dignity and respect is crucial. Observing this situation has made me realise just how important learning how to communicate well is and this is something I will strive to achieve throughout my career.
|
|
|||||||||||||||||||||||||||||||||||||||||||||
|
Throughout my time in the Caribbean I have witnessed the presentation and treatment of tropical diseases that I would not have done in the UK. I have seen patients with rheumatic fever, sickle cell disease and many strains of Tinea. The rarity of these conditions in the UK motivated me to learn about them whilst out in the Caribbean. It was useful to relate the written textbook presentation of these illnesses to a real life scenario. I now feel that I have gained more knowledge of tropical illness and disease through firsthand experience of the conditions. Conclusions Experiencing healthcare provision in a completely different and diverse setting has been a highlight of my training so far. I wanted to gain a perspective on how healthcare is provided in developing countries and how it encompasses the culture and beliefs of patients and doctors. I feel that this has been successfully achieved. Through observation and involvement with the doctors who are providing the care in these countries I learnt about their attitudes to health. I was also able to gain an insight into the structure of their healthcare system in each country and compare this to the structure in the UK. Having the opportunity to learn about a culture that is very different to our own has been a vital part of this experience. I now feel more confident in dealing with patients in hospital who may be from a different culture or religious background to my own. I learnt to respect and adopt their culture during my time abroad, an aim that I wanted to achieve. In conclusion, the experience of another countries healthcare system has been challenging yet rewarding. It has shown to me just how advanced healthcare provision is in the UK and how lucky we are to receive such good healthcare and modern facilities. I have learnt about barriers to healthcare provision in a developing country and the challenges that doctors in those countries experience. References
1. Discover
Jamaica, Geography
2. Hand
Hygiene. Use of alcohol rubs between patients: they reduce the
transmission of infections. BMJ 2001. August 25;323(7310):411-412 3. Global Aspects of Infection Control, Mary D. Nettleman, Infection control and hospital epidemiology, Vol. 14, No. 11, (Nov 1993), pp 646-648 4. Incidence and Prevalence of Diabetes in the Americas, Alberto Barcelo and Swapnil Rajpathak, Rev Panam Salud Publica/Pan Am J Public Health 10(5), 2001. 5. Rheumatic Fever, pp76-77, Clinical Medicine, Kumar and Clarke, 2005 Elsevier limited
6. An
overview of Laminar Flow Ventilation for operating theatres,
Queensland Health, October 1997.
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Dear Colleagues, Progress report from one of our bursary recipients - Leila Bassir
You will be aware that over the last two
years it has been resolved to use the income from the
Kidderminster Post Graduate Medical Centre Trust Funds to
support two £3,000 bursaries per annum. To date these have been
awarded to post graduate students in the first year of their
accelerated course in medicine. At the completion of this first
year, these bursary recipients have been asked to submit a
progress report and it was agreed at the Society's AGM earlier
this month that these reports should be published on our website
with the approval of the individual concerned. Hence, I am happy
reproduce the letter from Leila Bassir which I hope you will
find of interest.
Martin Lewis, Chairman of Trustees.
Letter received from Bursary recipient November 2009 Dear Dr Lewis
Well, finally my first year has come to an end, and as requested, I would like to write and thank you for the bursary granted to me last year, and tell you a little about how I am getting on here at Swansea Medical School. So, firstly, may I thank you most sincerely for accepting me for and granting me the graduate bursary last year, as my parents were both affected by the economic downturn, it was a great help not just for myself, but also a relief of pressure for them. My first year at Swansea has passed very well. I thoroughly enjoyed every moment of the course, and am very pleased with my exam results. As I wrote at the beginning of the year, anatomy has continued to be my most enjoyable subject, though unfortunately it is no longer on our curriculum, but neuroscience has taken its place as the next! Throughout I have found myself helped by the knowledge gained through my previous degree, which fortunately covered a lot of ground in clinical skills, and as we have now begun our ward visits, I have a chance to hone them upon actual patients.
This year has begun with quite a jolt compared to the last and
promises to be an interesting one. Last week, within the space of
48 hours, in fact, I found myself the Prince’s Foundation for
Integrated Health Student Network Champion for Swansea, and I only
replied to the email out of curiosity! Besides this, together with
my colleague and selected champion for the Cardiff branch of our
course, we are hoping to build an integrated health network within
the university itself, working with both staff, students, medical
and CAM professionals. Below is a list of the aims and objectives
for our intended project: As part of this project we hope to find speakers to discuss the use of CAM and integrated medicine, including both lay and qualified practitioners in order to provide an insight into the spectrum of usage likely to be encountered, and hopefully, medical practitioners who use CAM or practice integrated medicine. Our main goal, not to create an argumentative rally of should it be used or not, but fostering the fact that as doctors, we will encounter patients using other therapies and as such it is best that when faced with a ‘what do you think, Doc?’ that we know a little of what they are talking about. Besides the above project, I have also been involved in the creation of a new Medical School students’ magazine, both as lead typographer and contributor, and I would have included a first copy, but some of the authors made a decision to alter articles last minute, whilst I was unfortunately not around. My name is still on the page as typographer, however, so if you would like a copy, ... I didn’t do it! Right now, although I am enjoying everything, I still have no idea what I would finally like to do. I started off torn between rural GP, cardiology, neurology or surgery. Half way through, I had doubts on the surgery. Currently, it stands at GP, neurology or anaesthetics, whilst a lot of my colleagues say they can see me as general practitioner. I do know, that I would like to be able to combine a little minor surgery into general practice, so A &E or rural GP are top of the list. I still have several years though till the final decision, and I am sure our ward placements this year, and our two years clinical in Cardiff should help me make up my mind; and, four years ahead is a very long time, whilst, four years previously, I had no idea I would even be contemplating studying medicine! Once again, may I pass my greatest thanks, Sincerely, Leila Bassir
click to go to Index at top of page
|
||||||||||||||||||||||||||||||||||||||||||||||
|
Please click here to go back to the main website
|
||||||||||||||||||||||||||||||||||||||||||||||









.jpg)

